
A cost-effective at-scale early childhood development intervention integrated into existing public service infrastructure led to positive impacts on child development in Bangladesh
A growing body of research highlights the importance of early childhood development (ECD) in human capital formation (Knudsen et al. 2006, Almond and Currie 2011, Black et al. 2017). Early life investments are especially important for low- and middle-income countries (LMICs), since missing early investments can lead to lower human capital accumulation and intergenerational transmission of poverty.
An important policy challenge for LMIC governments is to find sustainable ways to implement effective ECD programmes at scale. The delivery of large-scale quality ECD interventions, however, imposes demanding infrastructure and personnel requirements to reach all parents and children in both urban and rural areas.
Leveraging existing service-delivery platforms to scale ECD interventions
One solution is to integrate ECD programmes into the existing public service infrastructure (Richter et al. 2017). The main advantages of this approach are: (i) economies of scale, (ii) demand and supply-side complementarities, and (iii) reductions in per-child costs of programme provision. However, there are potential downsides. First, challenges with programme delivery (such as distribution of programme materials) can dilute programme impacts (Araujo et al. 2021). Such declines in effect - or “voltage drops” - when scaling up have been documented in other settings (List et al. 2021, List 2022). Second, service providers may reallocate time away from their regular duties and towards the additional tasks, potentially worsening child outcomes in areas that the intervention does not target directly. This can be particularly salient when these providers are not offered compensation for the additional duties.
Integrating an ECD intervention into Bangladesh’s National Nutrition Services
The Bangladesh government runs the National Nutrition Services (NNS) programme that promotes best nutritional practices through micro-nutrient supplements, growth monitoring, and counselling support through monthly home-visits by community health workers. This NNS public health infrastructure presents an opportunity to integrate an ECD programme and deliver it at scale. The intervention we study was implemented by Save the Children, an international humanitarian aid organisation for children.
The intervention was delivered at scale, targeting more than 18,000 children aged 3-18 months in 78 community-clinic catchment areas across three out of seven divisions in Bangladesh (namely, Barisal, Chittagong, and Sylhet). Half of these catchment areas were randomly assigned to the treatment group which received the integrated NNS and ECD programmes, while the other half only received the pre-existing NNS programme. The ECD programme was a bundled intervention comprising the following components: (i) training of NNS workers on ECD, (ii) provision of four programme materials to parents, including a child development card with information on age-appropriate stimulation practices, two picture books, and a booklet with key messages and clinic visit guidelines, and (iii) regular ECD counselling during routine monthly visits by NNS workers. We did not provide any additional financial incentives to these workers.
Beliefs and behaviours of service providers
The training increased the perceived importance of ECD among service providers in the treatment communities. Service providers in the treatment group were more likely to report that it was important to teach mothers how to talk with children, respond to children's cues, and play games with their children.
In terms of behaviour, NNS workers in the treatment group spent approximately three more minutes per household visit discussing ECD, on a control group base of about two seconds. However, there was no significant impact on the total time spent with households. Effectively, these workers reallocated the time spent with parents by partially substituting away from discussions of child health and nutrition to spend more time on ECD. This result mirrors recent work by Berry et al. (2021), who find that a new nutrition intervention that distributed a micronutrient mix to be added to school meals crowded out a pre-existing school-based nutrition programme in Odisha, India.
Intervention impacts on child cognition, language, and socio-emotional skills
Figure 1
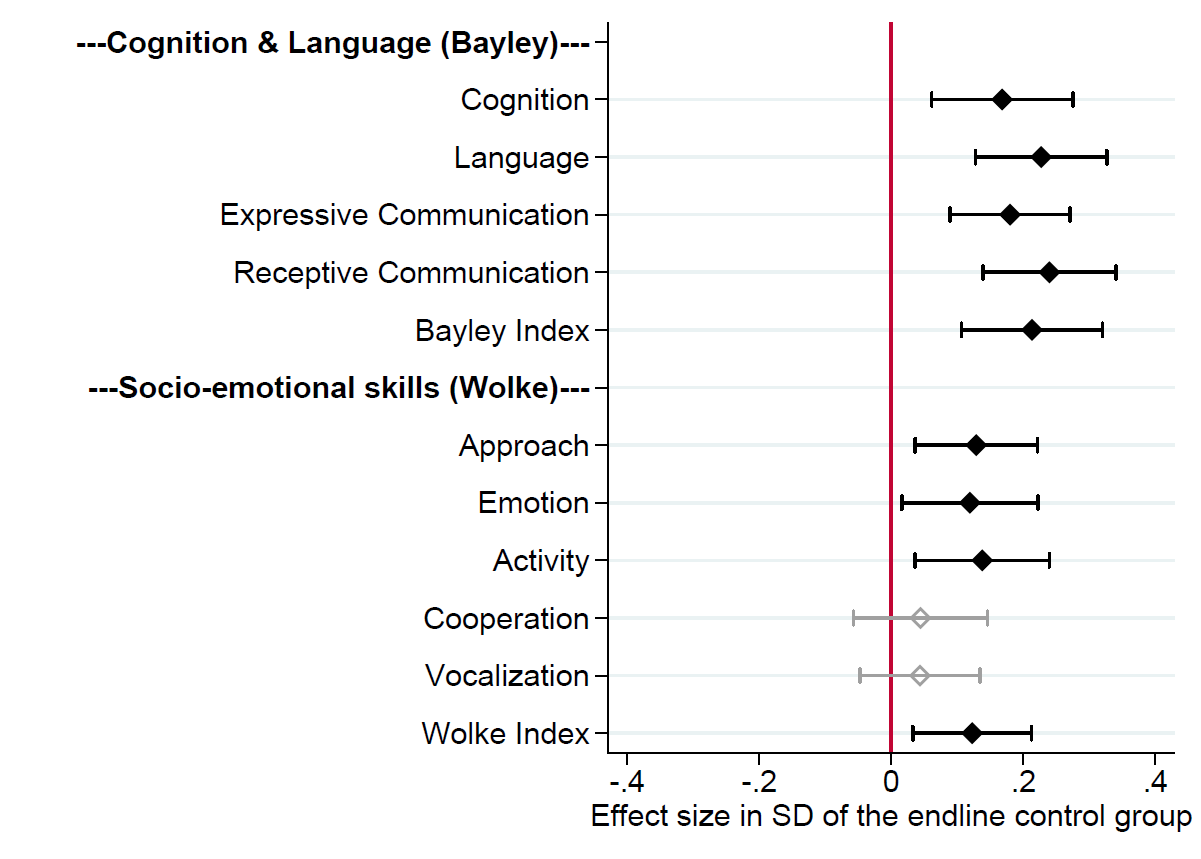
We summarise the intent-to-treat (ITT) effects of the intervention on our primary outcomes of interest in Figure 1, estimated using follow-up surveys conducted 1-3 months after the end of all intervention activities.
The intervention had positive and statistically significant impacts across all measures of child cognitive and language development: cognition, language, expressive communication, and receptive communication. Across the five measures considered under the Wolke behavioural rating, we observe statistically significant increases for three outcomes: approach, emotion, and activity.
The reallocation of service-provider time away from child nutrition and towards ECD did not lead to adverse effects. We find better nutritional outcomes, with the intervention reducing wasting and underweight rates.
Mechanisms
Figure 2
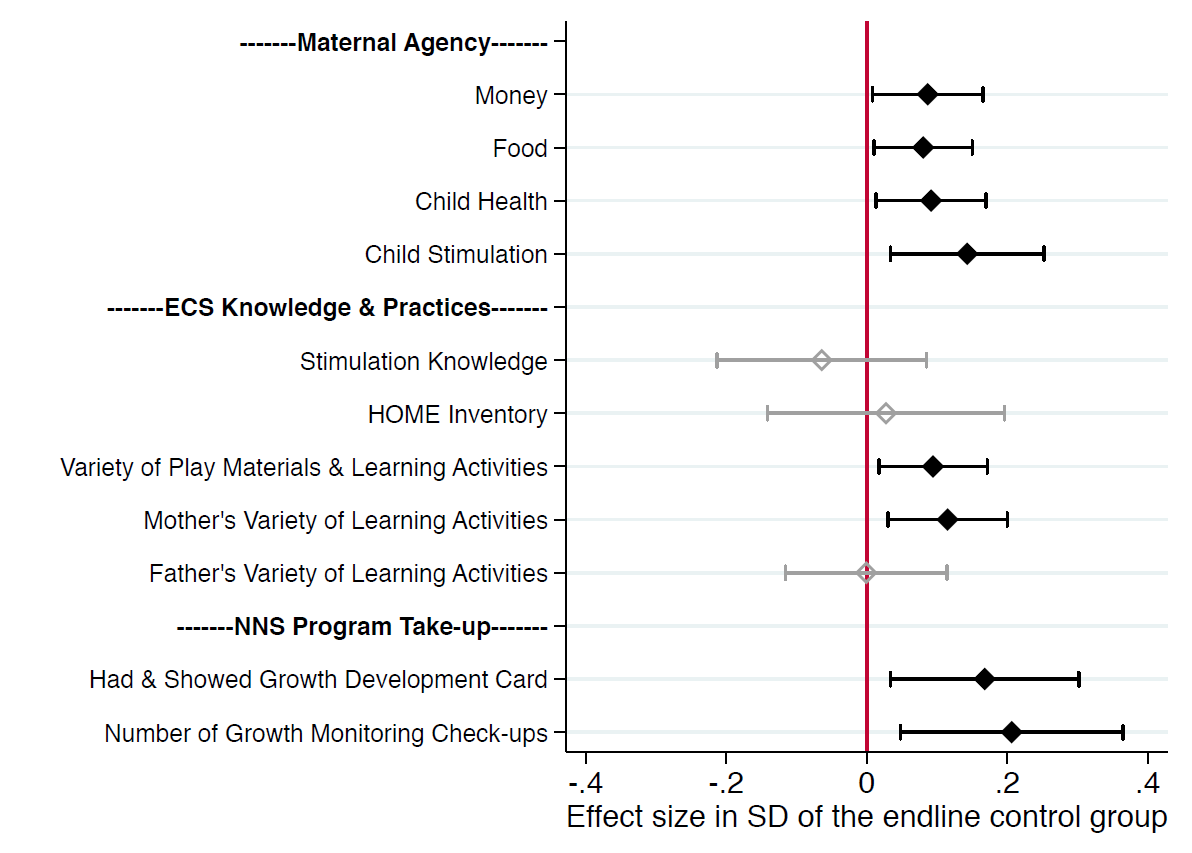
What are some mechanisms underlying the theory of change for the intervention, in addition to receipt of the programme materials and discussions with service providers? We consider three mechanisms: maternal agency, parental investments, and demand-side complementarities relating to take-up of the NNS programme. We find positive and significant effects on maternal decision-making agency, with larger effects in the domains of child health and stimulation. Mothers in the treatment group also scored higher on the variety of play materials and learning activities that they offered to the child. Lastly, we see that households in the treatment group were more likely to have and show the NNS growth development card, and children in the treatment group took up more NNS growth-monitoring check-ups.
Cost-benefit analysis
As developing countries weigh the cost-effectiveness of various poverty alleviation strategies, understanding the rates of return to early childhood programmes can have important policy implications for how governments choose to spend scarce resources.
We estimate that the cost per child was around USD 6.84. These costs are low given that the intervention relied on existing NNS infrastructure and service providers. The potential long-term benefits of the programme include an increase in wages arising from improvements in cognitive and non-cognitive skills. We convert the estimated treatment impacts into wage gains using estimates from the literature and compare them with the costs to compute an internal rate of return of 18.9%. This is significantly larger than the rates of return to ECD programmes implemented in other countries.
Discussion
The synergies that we uncover, particularly relating to demand-side complementarities, complementary parental investments, and improved maternal agency, are of substantive public policy importance. Such synergies allow for the cost-effective integration of services that would be attractive for governments working to implement such programmes at scale. The lack of detrimental crowding-out effects, a concern with integrated programmes, further reinforces the benefits of these synergies while minimising their costs. However, we must caveat our findings by emphasising that we worked in the context of an existing nutritional intervention. The ECD programme may have had different effects if it was rolled out independently or by riding on a non-nutritional baseline intervention.
The challenges of at-scale delivery remain, however. As per the intervention guidelines, households in the treatment group should have received four materials: a child development card, a household picture book, a nature picture book, and a key message booklet. But, only half of the households in the treatment group received any three of these four materials. Compliance is strongly negatively correlated with distance, or time to the nearest clinic. Further work is needed to understand the challenges pertaining to compliance of at-scale programme delivery.
Editor's note: The order of authors has been randomized using the Author Randomisation Tool of the American Economic Association.
References
Almond, D and J Currie (2011), “Human Capital Development before Age Five,” Handbook of Labor Economics, 4b(15): 1315–1486.
Araujo, M C, M Rubio-Codina and N Schady (2021), “70 to 700 to 70,000: Lessons from the Jamaica Experiment,” in “The Scale-Up Effect in Early Childhood and Public Policy,” Routledge, pp. 211–232.
Berry, J, S Mehta, P Mukherjee, H Ruebeck, and G K Shastry (2021), “Crowd-out in school-based health interventions: Evidence from India’s midday meals program,” Journal of Public Economics, 204: 104552.
Black, M M, S P Walker, L C H Fernald, C T Andersen, Ann M DiGirolamo, C Lu, D C McCoy, G Fink, Y R Shawar, J Shiffman et al. (2017), “Early childhood development coming of age: science through the life course,” The Lancet, 389(10064): 77–90.
Bos, J, A Shonchoy, S Ravindran and A Khan (2023), “Early Childhood Human Capital Formation at Scale,” SSRN Working Paper 3906697.
Knudsen, E I, J J Heckman, J L Cameron and J P Shonkoff (2006), “Economic, neurobiological, and behavioral perspectives on building America’s future workforce,” PNAS, 103(27): 10155–10162.
List, J A (2022), The Voltage Effect, Crown Publishing Group.
List, J A, D Suskind and L H Supplee (2021), The Scale-Up Effect in Early Childhood and Public Policy, Routledge.
Richter, L M, B Daelmans, J Lombardi, J Heymann, F Lopez Boo, J R Behrman, C Lu, J E Lucas, R Perez-Escamilla, T Dua, Z A Bhutta, K Stenberg, P Gertler, G L Darmstadt, Paper 3 Working Group, and The Lancet Early Childhood Development Series Steering Committee (2017), “Investing in the foundation of sustainable development: pathways to scale up for early childhood development,” The Lancet, 389(10064): 103–118.




