
Governments commonly use school infrastructure to implement programmes targeting child health, but additional programmes can overwhelm administrative capacity and crowd out the delivery of existing programmes.
Editor's note: Figure 2 was updated to correct an error with the standard error bars.
Schools around the world are often relied upon to provide services to children beyond education. In particular, governments rely on school infrastructure to implement programmes aimed at improving child wellbeing, such as health interventions (Bundy et al. 2018). In 2018, the World Health Organization and UNESCO launched the “Making every school a health-promoting school” initiative aimed at improving the health and wellbeing of students and families by “capitalizing on the organizational potential of schools.” With growing focus on the potential of schools to improve the wellbeing of children such as commitments for delivery of school meals, it is increasingly important to understand how school-based interventions can be more effectively implemented (Finan et al. 2017). Our study evaluates the impact of introducing additional programmes on the implementation of existing programmes and suggests that using existing school infrastructure comes with important hidden costs. Even when new programmes are designed to complement existing programmes, they may actually crowd each other out.
As part of a randomized controlled trial in Odisha, India, we measured the impacts of introducing a novel nutrition programme and a monitoring intervention on the implementation of a pre-existing school-based nutrition programme (Berry et al. 2021).
Previous work has found monitoring to improve performance of school officials (see e.g. Duflo et al. 2012). We also examined how the interaction of these various interventions affected the main outcome of interest, child health.
Pre-existing school-based nutrition programmes in India and the role of school staff
Since 1995, the Indian Government’s Midday Meal Scheme has aimed to improve the nutrition of school-aged children by providing nutritious cooked meals in school. In the schools in our sample in Odisha as in other states in India, the headmaster was responsible for purchasing food materials, obtaining cooking fuel, and hiring and supervising cooks.
More recently, in 2012 India’s Ministry of Health and Family Welfare launched an iron and folic acid (IFA) supplementation programme to reduce the prevalence and severity of anaemia among school aged children. Beginning in January 2013, weekly iron and folic acid supplements as well as a semi-annual deworming medication were distributed to all students attending public schools. In our school sample, headmasters received the tablets, assigned a teacher to be in charge of IFA implementation, and supervised the provision at school.
The design of our study
As part of our study, we implemented two interventions:
- The provision of a micronutrient mix (MNM) to be added to the school meals. The mix was intended to improve absorption of iron from the iron supplements, thereby complementing the government’s IFA programme (Best et al. 2011).
- High-intensity monitoring, intended to improve the programme’s implementation. All schools received lunch-time visits to monitor programme implementation during the last 3 months of the intervention, but the high-intensity schools received additional visits in the first two months of the intervention.
The study was conducted in 148 schools in Odisha, India, all of which were within 50 kms of Kendujhar, the administrative headquarters of the district. The schools were randomised into four groups that allowed us to estimate the effects of 1) the micronutrient mix, 2) the degree of monitoring intensity, and 3) interactions between the two. Specifically, out of the 148 schools in the sample, 38 were randomly assigned to receive the MNM intervention without high intensity monitoring, 36 received high intensity monitoring without the MNM intervention, 37 received both the MNM intervention and high intensity monitoring, and 37 received neither intervention, serving as a comparison group. Table 1 presents the number of students enrolled and the number of students surveyed at the end of the intervention in these four groups of schools.
Table 1: Distribution of students among treatment groups
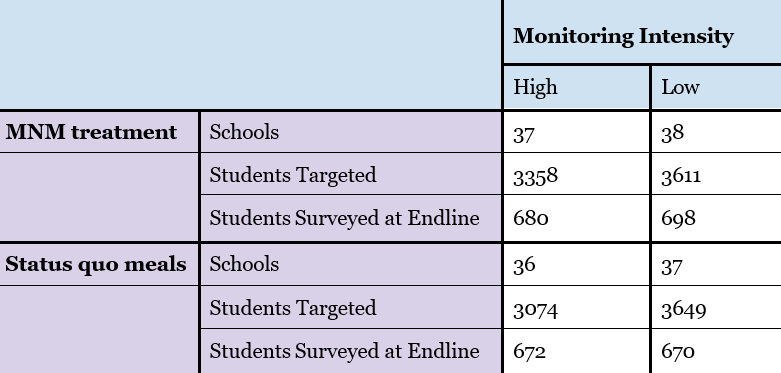
Notes: This table presents the number of schools, students enrolled, and students surveyed in each of the four treatment groups.
Figure 1 presents the chronology of key activities in the study. Panel A shows a timeline of the entire study. The MNM and high-intensity monitoring treatments were introduced at the end of November 2014 and continued through April 2015. After the intervention (between April and July 2015), we conducted a household survey in which we measured child haemoglobin levels. We also collected data on school resources such as staffing and infrastructure.
Panel B describes the data collected during the intervention period from December 2014 to April 2015. High intensity monitoring schools started receiving monitoring visits from the very beginning of the programme, whereas low intensity monitoring schools began receiving these visits in the third month of the intervention. These monitoring visits were fairly comprehensive; enumerators spoke to the headmaster and cook about the preparation of the meal, collected a sample to be sent to the lab for nutritional testing, and observed the amount of food distributed to and consumed by randomly chosen children. In addition, enumerators visited all schools during the first, third, fourth and fifth months to survey headmasters about the implementation of the pre-existing IFA programme and interviewed three randomly chosen students about whether they regularly received IFA tablets in school.
Figure 1: Chronology of study activities
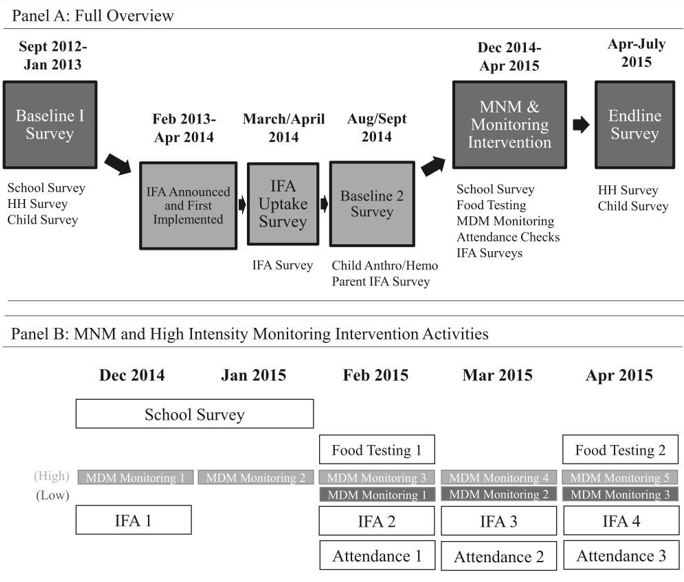
Notes: This figure presents a timeline of the key activities during the study overall (Panel A) and the data collection activities during the five-month intervention period (Panel B).
New programme crowds out existing programme implementation
Figure 2 presents the impact of the interventions, by comparing the three treatment groups of schools to the comparison group of schools that did not receive the MNM or the high-intensity monitoring visits. The three outcome variables are indicated by colour: green depicts differences in the proportion of children who are anaemic, the main outcome of interest; yellow indicates differences in the proportion of children who report receiving tablets in school weekly, a measure of the take-up of the government’s IFA intervention; and blue indicates differences in the amount of nutrients present in meal samples, a measure of take-up of the MNM intervention. Grouping together the three outcomes, from left to right, Figure 2 displays the impact of only receiving the MNM mix, the impact of only receiving high-intensity monitoring, and the impact of receiving both. The black lines indicate ninety-five percent confidence intervals.
Figure 2: Treatment effects by groups
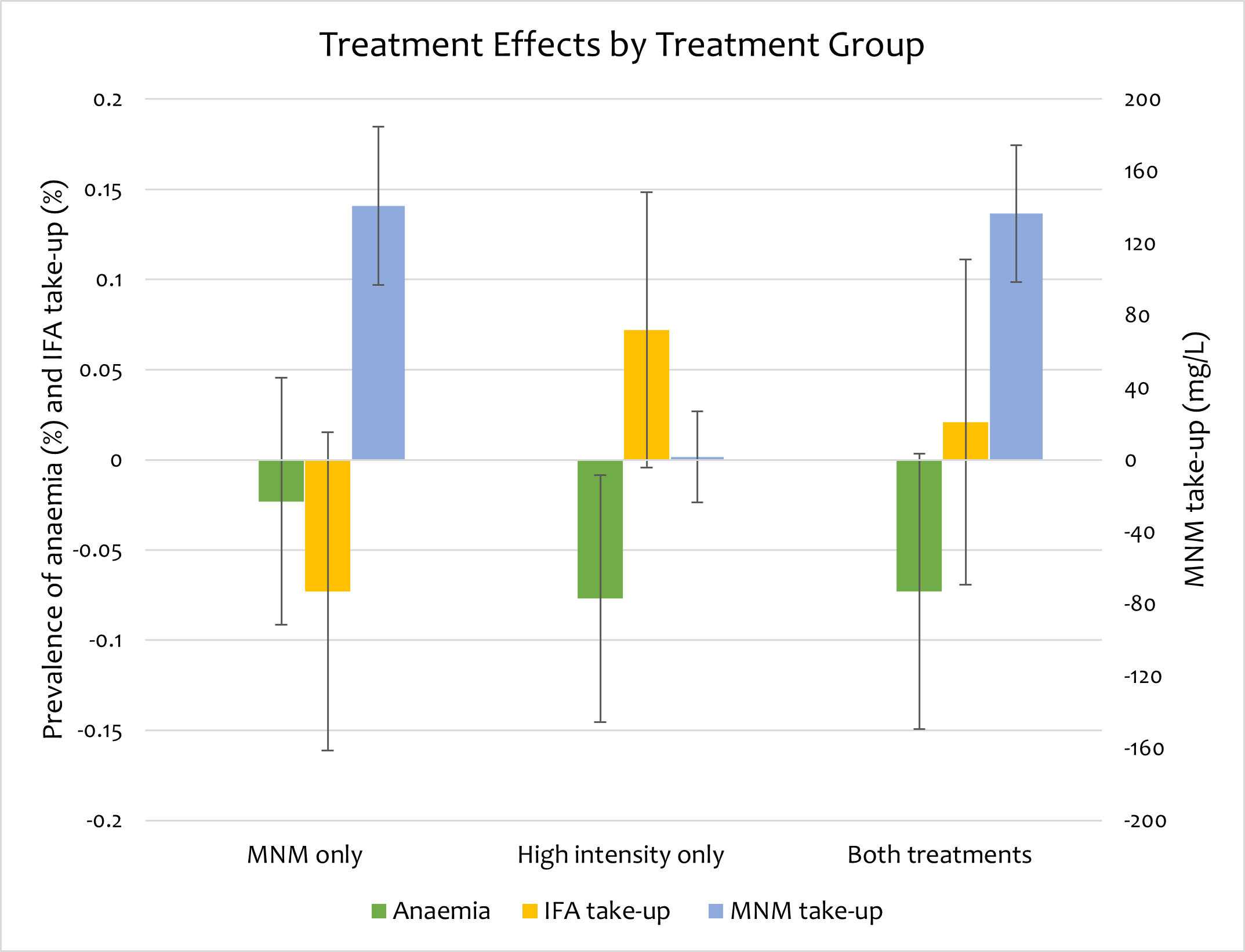
Notes: This figure presents the difference between the treatment groups and the comparison group that did not receive the MNM or the high-intensity monitoring visits for three indicative outcome variables to demonstrate the impact on child health (percent of children who are anaemic, defined as having haemoglobin concentrations below 11.5 g/dL, green bars), IFA program implementation (percent of children who receive tablets weekly, yellow bars), and MNM programme implementation (nutrient content in the meal samples, blue bars).
We found that introducing the MNM programme to schools crowded out the implementation of the government’s existing IFA programme.
- Students in the MNM-only schools were less likely to report receiving IFA tablets regularly.
- Despite substantial take-up of the MNM – nutrient content of the meals increased significantly – the MNM-only schools experienced no significant change in prevalence of anaemia as an indicator of child health.
Intense monitoring improves implementation and mitigates the crowding out effect
At the same time, we found that frequent monitoring visits without the MNM programme improved implementation of the IFA programme and, subsequently, child health.
- Students in the high intensity treatment arm were more likely to report receiving IFA tablets regularly.
- Increased monitoring of schools significantly reduced the prevalence of anaemia.
In fact, the crowd-in effect of frequent monitoring alleviated the crowd-out effect of the MNM intervention.
- Students in schools that received both interventions did not experience a significant change in IFA take-up.
- In these schools, the greater nutrient content in school meals had their intended effect of reducing anaemia prevalence and improving child health.
These results reaffirm that frequent monitoring can improve implementation of public health programmes, and is perhaps even a necessary component of any programme newly layered onto existing infrastructure.
In addition, we provide suggestive evidence that the crowd-out and crowd-in impact on IFA tablet distribution depends on the administrative capacity of the school. Crowd-out of the IFA programme by the MNM programme, and crowd-in of the IFA programme by monitoring, are predominantly found among schools that appear more resource-constrained in their staffing and meal funding. This is particularly true in schools with an above-average number of students per staff member.
Implications for policymaking
Our study shows that utilising school infrastructure to deliver health programmes remains a promising strategy to improve the health and well-being of children in developing countries. However, there is a need to exercise caution when designing these programmes. Layering on additional programmes without considering administrative capacity constraints can hinder implementation of other non-educational programmes and perhaps even sacrifice educational quality. In contrast, increasing external monitoring not only improves programme implementation, but we find that it reduces the risk of crowd-out.
Our study shows that when designing new school-based programmes, policy makers should consider interactions with existing programmes and provide additional resources for monitoring. This can improve the implementation, and thus efficacy of both existing and new programmes.
References
Berry, J, S Mehta, P Mukherjee, H Ruebeck, and G K Shastry (2021), “Crowd-out in school-based health interventions: Evidence from India’s midday meals program”, Journal of Public Economics 204: 104552.
Best, C, N Neufingerl, J M Del Rosso, C Transler, T van den Briel, and S Osendarp (2011), “Can multi-micronutrient food fortification improve the micronutrient status, growth, health, and cognition of schoolchildren? A systematic review”, Nutrition Reviews 69: 186-204.
Duflo, E, R Hanna, and S P Ryan (2012), “Incentives Work: Getting Teachers to Come to School”, American Economic Review 102(4): 1241-1278.
Finan, F, B A Olken, and R Pande (2017), "The personnel economics of the developing state", Handbook of Economic Field Experiments 2: 467-514.





