
Private care led to large savings for the public sector and improved health outcomes through more access to care, not necessarily better technology
The optimal mix of public and private healthcare has witnessed considerable debate the world over. Most countries feature universal or near-universal public provision of either health insurance or direct healthcare to residents. In all of these countries, this public provision is to some extent supplemented by private options.
Diabetes is a chronic non-communicable disease that is strongly associated with being overweight and obese, and is one of the most pressing public health problems facing developing countries. In 2019, there were 4.2 million deaths from diabetes-induced complications in the world. Although this disease is not curable, it can be controlled through constant monitoring and with the provision and support of relatively inexpensive medicines.
Public and private healthcare in Mexico to treat diabetes
The prevalence of diabetes in Mexico has increased from 6.7% in 1994 to 11% in 2018, causing significant saturation of public health services. Diabetes has been the second most common cause of death in Mexico and is amongst the top five causes of disability. Mexico spends enormous amounts to combat this disease: the estimated costs to address diabetes and its consequences are 2.2% of GDP. The lion’s share of spending on diabetes treatment (87%) is on ensuing complications; as a result of poor diabetes control, with the rate of hospital admissions almost double the average in OECD countries. The main approach adopted by Mexico to address the health consequences of diabetes is through its public health systems; the Instituto Mexicano del Seguro Social (IMSS), for example, covers 70.3 million workers in the formal sector and their families, and cares for about 4.7 million diabetics each year. In Mexico, as a consequence of large waiting times, a private sector has emerged to provide complementary primary care. The proportion of private medical offices increased from 5% in 1990 to more than 30% in 2020. In 2018, almost 20% of diabetics reported receiving treatment in private institutions (INSP, National Health and Nutrition Survey 2018).
Given the large human and fiscal costs of this disease, it is essential to understand the implications of private alternatives and whether they can play a role in providing early care to help avoid complications. Yet, in Mexico and in the world, there is little evidence in this regard. Evaluating the impact of private alternatives faces several challenges: use of private providers is endogenous and randomised trials are also difficult given the enormous samples needed to obtain sufficient first-stage power.
In a recent study (Bronsoler, Gruber, and Seira 2021), we evaluate whether increasing access to private health providers to treat diabetes has benefits for the population. We find a strong complementarity between both sectors and conclude that cooperation between the public and private sectors to increase access to early diabetes care would present a significant improvement in health status, along with additional savings for the government driven by averted complications.
Deniers randomisation to causally estimate the effect of private healthcare
We implement a novel deniers randomisation approach (screenining out individuals who would enrol even without a subsidy) to cost-effectively provide a causal estimate of enrolment in private diabetes care. We run this experiment in partnership with a private provider of comprehensive diabetes care in Mexico, Clinicas de Azucar (CdA) with support from Eli Lilly and Company. CdA’s service costs 7000 pesos (US$350) per year, or 5% of the median Mexican family yearly income. Our initial sample comprises individuals who undergo a free initial comprehensive diabetes evaluation at CdA, which we randomise into treatment and control groups, and survey at baseline. After their evaluation, these individuals are offered the opportunity to enroll in CdA at full price, with 31% doing so. Amongst those who decline and are willing to hear additional offers, an additional opportunity to enroll at 40% of the baseline price is presented to the treatment groups but not the control. Amongst those offered this discount, 49% end up using the CdA service, compared to 21% enrolment for the control group that does not get this offer. This provides a powerful first stage to investigate the impact of CdA treatment in a cost-effective way. We estimate costs that are one-tenth of what they would have been if we had randomised amongst all those who went for the evaluation.
Figure 1 Deniers randomisation sample size savings
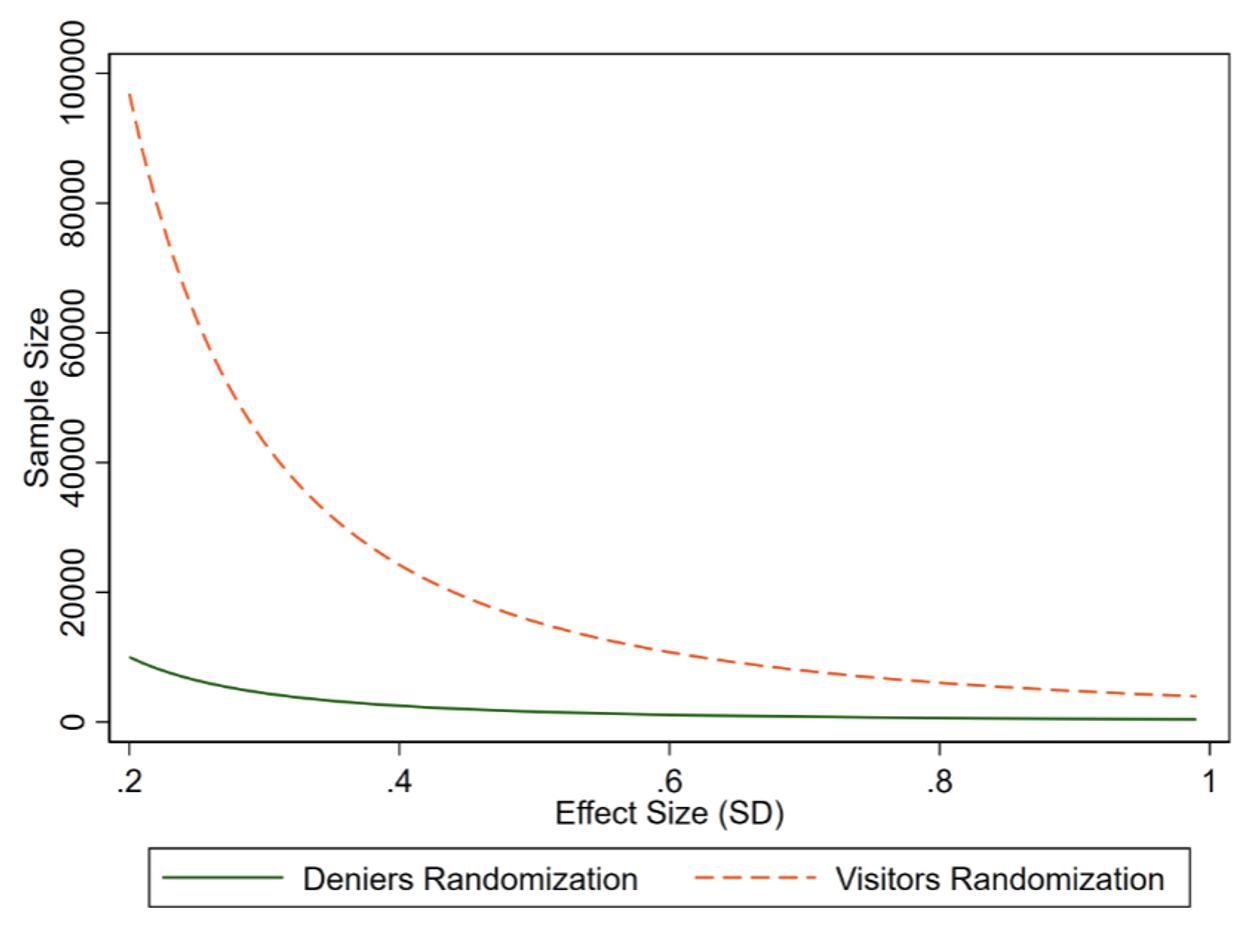
Notes: This figure shows the sample needed to detect an effect with 80% power and an 5% confidence under “Visitor’s randomisation” vs “Deniers randomisation”. Visitors’ randomisation would involve randomising to treatment subsidy or control all those who arrived at CdA for a free screening. “Denier’s randomisation” consists of screening out always takers and/or never takers from the sample. Under some (weak) assumptions, we can estimate the same LATE that would be estimated with visitor’s randomisation, but with a fraction of observations needed to achieve a given statistical power.
Effects of the CdA intervention
Using this approach, we find a large effect of the CdA intervention: the implied effect of participation is to lower blood sugar levels (measured by glycated hemoglobin or HbA1c) by a full point (relative to a control mean of 8.5%), and to increase the share of those treated who are under control by 69%. This is a huge impact, which according to the widely cited UKPDS study, could reduce microvascular diabetes complications by 35%. Moreover, this impact is at the upper end of estimated effect sizes from other diabetes interventions reviewed in a recent meta-analysis (Pimouguet et al. 2011a). Along with the important effect on health, we find that having access to CdA has an important effect on adherence to treatment: patients go 35% more to the doctor, see more specialists, and follow their prescriptions better. They are also more likely to maintain their diet and exercise – behavioural factors that are important in managing diabetes. We find that diabetic complications fall, even in the short run.
Figure 2 Summary of effects of enroling in private care
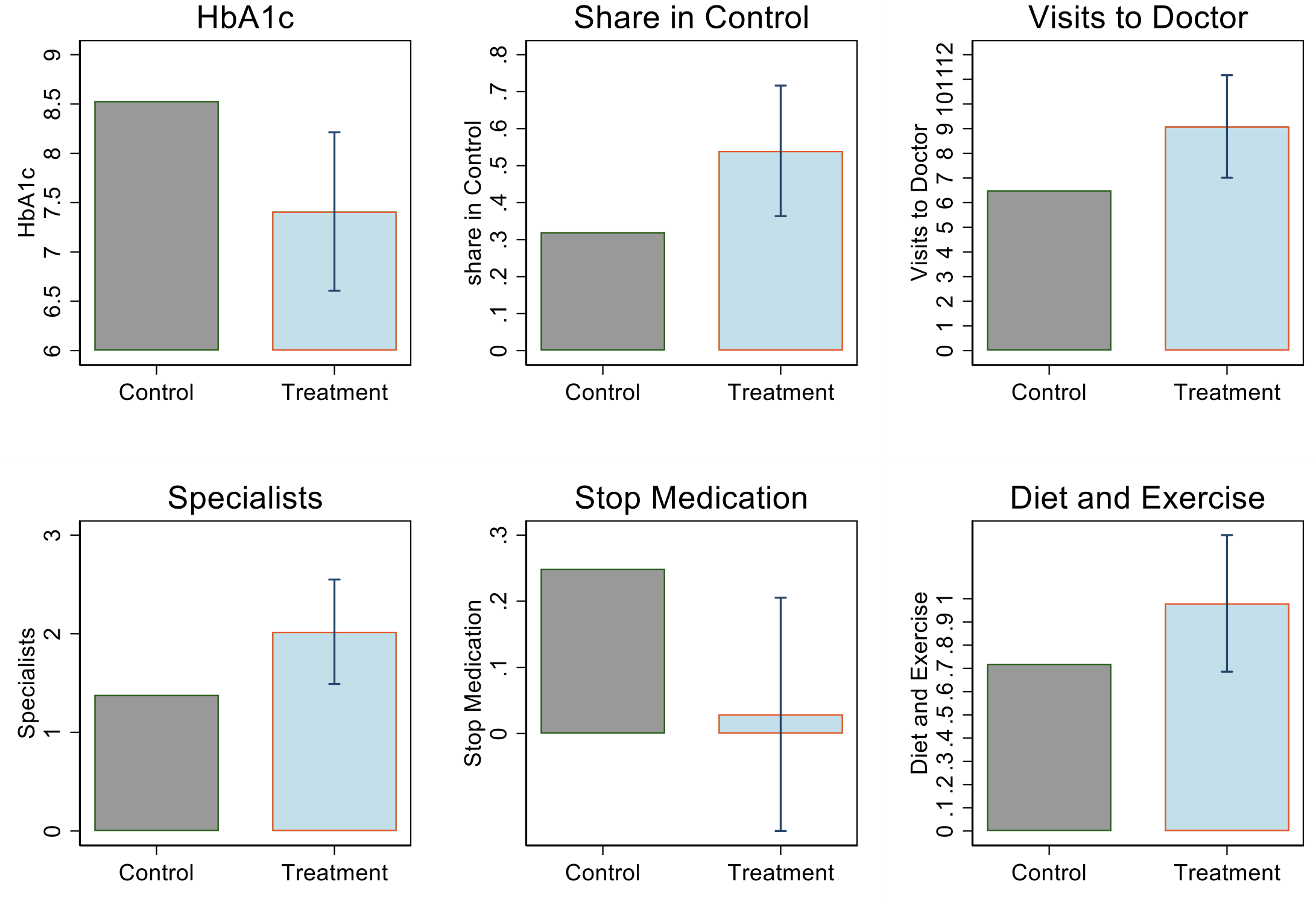
This figure shows the results obtained along with the 95% confidence interval. The control bar reports the mean among control group individuals while the treatment bar reports how the mean shifts with the effect.
To further consider the welfare implications of our results, we extend them in two ways:
- First, we explore the cost-effectiveness of the CdA intervention. The net costs of this intervention are much lower than the gross costs because of savings to the public health system. Healthcare in these private sector clinics has large positive fiscal externalities. On average, 55% of the costs associated with private care would be recovered in the expense of avoided complications, which is usually paid for by the public sector. If we add to this the fact that 40% of people with access substitute the public sector for the private sector as their main health provider, the programme produces enormous savings for the public sector. Adding these components, we estimate that the net benefit of this supplement in terms of money is between 65% and 105% of its gross costs. Finally, if we incorporate the cost of living of the deaths averted, the benefit of the programme is ten times its cost. In other words, this private care has a social value that far exceeds what was charged for it.
- Second, we assess whether these returns to private care reflect a more productive delivery of care per visit or simply more quantity of care that is delivered equally effectively. We use data from the major public sector insurer (IMSS), along with variation coming from the distance to public clinics, to quasi-experimentally estimate the marginal returns per visit to IMSS diabetes care. We find that after controlling for differential observable selection into private sector care, the returns to public and private care per visit are in fact comparable. This suggests that the returns from CdA reflect the ability of the private vendor to encourage more care. We confirm this conclusion by showing that our treatment effects are in fact highest where public clinics are most crowded.
Contribution to existing literature
Our findings contribute to the long-standing discussion on public versus private healthcare provision. In a systematic review of the literature, Basu et al. (2012) document that the private sector is usually not more efficient, accountable, or medically effective than the public sector but offers better waiting times and hospitality towards patients. Das et al. (2012, 2016) document through standardised patient comparisons in India that both the public and private sector offer similar (low) quality services, with public sector physicians being more prepared but private sector practitioners compensating with more effort per appointment. In the US, two recent studies evaluate the role of private options relative to healthcare for the nation’s military and veterans, with mixed outcomes. Frakes et al. (2021) find that children of military personnel born in the private sector have higher costs but better outcomes than those born on military bases, while Chan et al. (2020) find that those receiving emergency care at Veterans Administration hospitals experience both lower costs and better outcomes. We contribute to this literature by showing that there is a large health benefit of adding a (subsidised) private option, even for those with free public healthcare, and even if the private option is not necessarily of higher quality per unit of delivery. This is especially true in a context where public healthcare is overstretched. Next, we run one of the largest double-blind diabetes field experiments to date and show that standard diabetes care with simple and cheap technology can have an enormous impact on reaching normal sugar levels. Finally, we show that large fiscal externalities pay manyfold for the subsidy we implemented, contributing to the literature on fiscal externalities from health interventions (see Chandra et al. 2010 for a review of this literature).
Private delivery of diabetes care has substantial benefits
Private care in Mexico led to improved health and significant offsets to public sector hospital expenditures, and was highly cost-effective at standard values of improved health. The source of the improvements, however, was not necessarily better technology for diabetes care, but rather encouraging more care and enabling greater access to it. It is likely that the public sector itself, by improving access to care for its members (waiting times, distance to clinics, and customer experience), could improve preventive health for diabetics and avoid complications. Alternatively, or in tandem, governments seeking to improve their diabetes care but with overcrowded public delivery, could test outsourcing care.
References
Basu, S, J Andrews, S Kishore and D Stuckler (2012), “Comparative Performance of Private andPublic Healthcare Systems in Low- and Middle-Income Countries: A Systematic Review”, PLOS MEDICINE 6.
Bronsoler, A, J Gruber and E Seira (2021), “The Impact of a Private Supplement to Public Health Care: The Mexico Diabetes Experiment”, NBER Working Paper 28913.
Chan, D, D Card and L Taylor (2020), “Is There a VA Advantage? Evidence from Dually Eligible Veterans”, Stanford University mimeo.
Chandra, A, J Gruber and R Mcknighy (2010), “Patient cost-sharing and hospitalization offsets in the elderly”, American Economic Review 100.
Das, J, A Holla, V Das, M Mohanan, D Tabak and B Chan (2012), “In Urban And Rural India, A Standardized Patient Study Showed Low Levels Of Provider Training And Huge Quality Gaps”, Health Affairs 31.
Das, J, A Holla, A Mohpal and K Muralidharan (2016), “Quality and Accountability in Health CareDelivery: Audit-Study Evidence from Primary Care in India”, American Economic Review 106.
Frakes, M, J Gruber and T Justisc (2021), “Public and Private Options in Practice: The Military HealthSystem”, NBER Working Paper 28256.
Pimouguet, C, M L Goff, R Thiebaut, J F Dartigues and C Helmer (2011a), “Effectiveness of disease-management programs for improving diabetes care: a meta-analysis”, CMAJ-JAMC 183.



