
Teaching women in Kenya to visualise alternative future scenarios based on current behaviour increased chlorination of drinking water, reduced children’s diarrhoea, and improved savings after almost three years
Individuals often fail to invest in preventive healthcare, even when such investments cost little and individuals are aware of their benefits. A prominent example is chlorination of drinking water, which is highly effective in reducing the prevalence of diarrhoea, particularly among young children. Diarrhoea is the second leading cause of death worldwide among children aged one to five, contributing to nearly half a million deaths in 2015. In many settings, chlorine for water is readily and cheaply available, but infrequently used by individuals without access to clean water. In our study areas in Kenya, only 3% of households used chlorine before any intervention, although a month's supply costs only 25 Kenyan shillings (equivalent to USD $0.25). Interventions which provide chlorine for free, often in combination with information or marketing campaigns, can increase usage, but take-up remains far from complete (Dupas et al. 2016, Null et al. 2018, Luoto et al. 2014, Dupas et al. 2020). This suggests a potential role for behavioural or psychological barriers: individuals may not value the future enough, relative to small hassle costs in the present. Alternatively, they may lack self-efficacy - i.e. the belief that their own actions can shape their future. Finally, they may face cognitive constraints, such as the ability to plan and organise chlorination.
In our recent research (John and Orkin 2022), we test if short workshops can (i) affect such psychological barriers and (ii) increase investment in health and other domains in the short- and long run.
Study setting and interventions
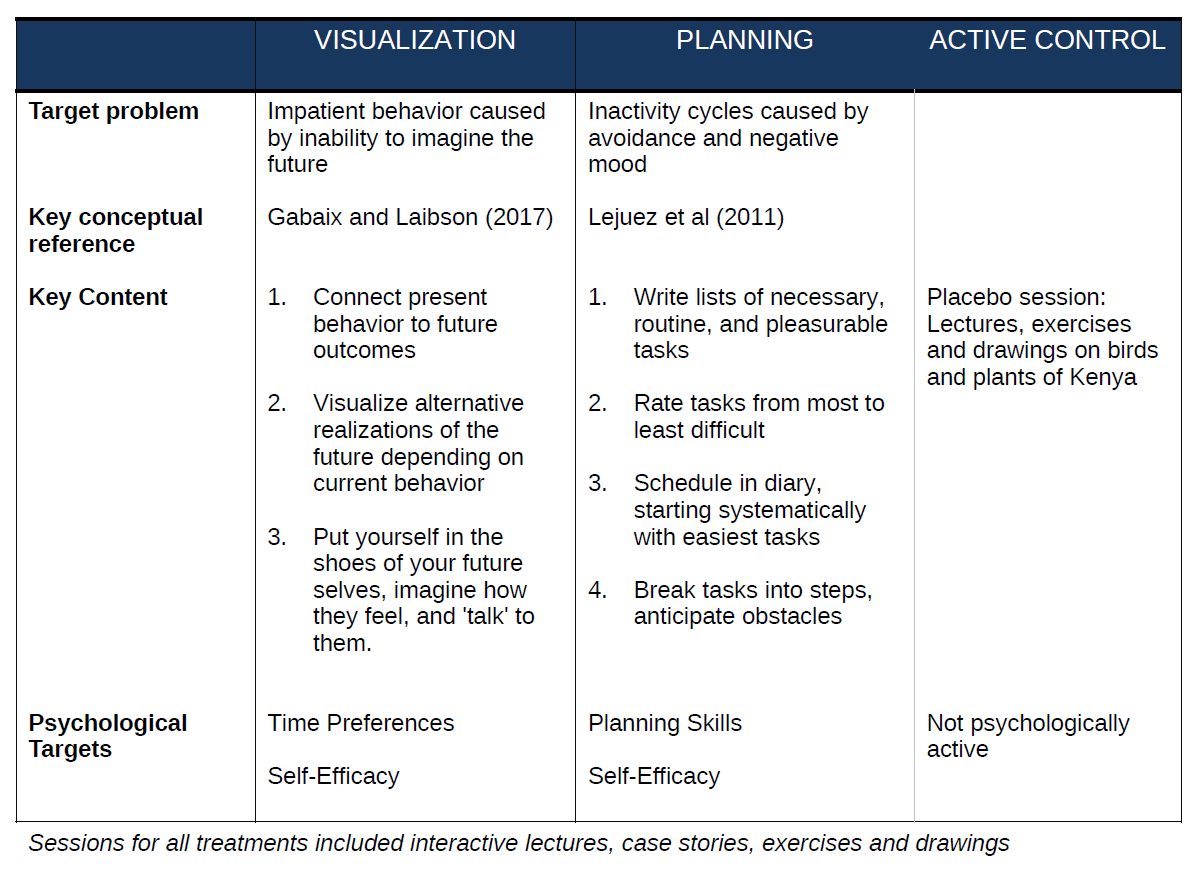
We conducted a randomised field experiment in rural Western Kenya (Bungoma and Kakamega counties). The study recruited 3750 women from 205 villages, aged 18-35 as this group is the most likely to have small children, who are the most vulnerable to diarrhoea. The intervention consisted of two-hour, two-session workshops, organised in groups of five in mobile laboratories. Women were assigned to one of four treatment groups:
- Visualisation: This intervention was motivated by insights from psychology and neuroscience that thinking about present or future rewards activate different systems in our brain. Put simply, we may be impatient because it is much easier to imagine the present, then it is to imagine the future. In these workshops, participants learned to visualise alternative realisations of the future, depending on their behaviour in the present. The approach was deliberately visceral, with participants putting themselves in the shoes of their ‘future selves,’ imagine how they feel, and `talk' to them. The intervention aimed to increase patient behaviour by making future outcomes more vivid and tangible in participants' minds, thus increasing their perceived value relative to the more immediate costs required to attain them.
- Planning: This intervention was adapted from a psychotherapy approach known as behavioural activation, which is based on the idea that people get stuck in vicious cycles of avoiding tasks, then feeling bad about this, and as a result having even less energy to start it. The workshops aimed to improve planning skills, helping participants to undertake activities that they were struggling to do regularly by making specific plans, and establishing routines. Both interventions required participants to think about how their current behaviour affects their future outcomes, and thus both needed and strengthened self-efficacy.
- Active Control: A third, active control group received placebo workshops, containing all elements of the intervention except the psychologically active components. Instead of psychologically active topics, they discussed the birds and plants of Kenya. In addition, all three groups received a short information module about the benefits of chlorination, in order to hold beliefs about chlorination constant across groups.
- Pure Control: A fourth, pure control group did not receive workshops. They were simply surveyed at endline.
Figure 1: Interventions
Main findings
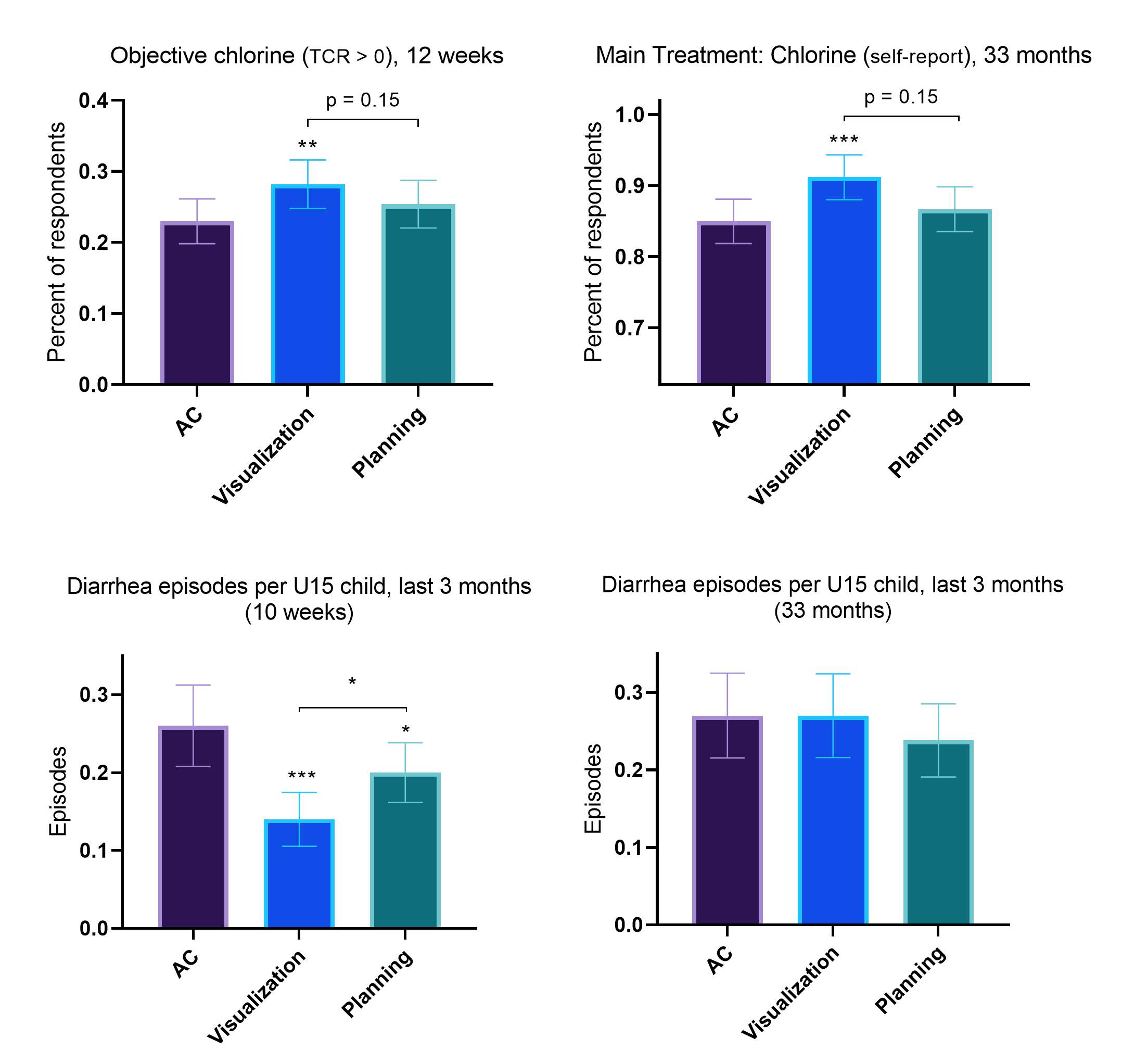
Twelve weeks after the intervention, we observe economically large and statistically significant effects of Visualisation on our main outcome of interest, objectively measured chlorination of household drinking water. Specifically, we find a significant increase of 22% (5 percentage points) in the share of households whose drinking water contains chlorine, relative to the active control group, twelve weeks after the interventions. Self-reports confirm this finding. We show suggestive evidence that this effect persists over time: after almost three years, when asked an unprompted question about how they treat their water, participants in the Visualisation group are 5 percentage points more likely to state that they chlorinate it. The number of diarrhoea episodes per child under 15 decreases by 46% (0.12 episodes) relative to the active control after ten weeks. This effect does not persist over time, although we show this may be due to differences in season between rounds. In contrast, the Planning intervention has positive but largely insignificant effects on health outcomes.
The Visualisation intervention is highly cost-effective, with a delivery cost of USD $4 per household, and a cost per Disability-Adjusted Life Year (DALY) saved between USD $62 and $248 depending on assumptions.
While our primary interest is in health, our interventions are domain-general in nature, and may thus reduce barriers to forward-looking behaviour in general. Indeed, we observe that the Visualisation intervention led to significant increases in savings. The effects persist after almost three years, allowing the Visualisation group to accumulate 41% higher savings balances. This savings increase was measured during the 2020 global pandemic, suggesting that participants who learned visualisation techniques in 2017 benefited from an increased financial buffer in 2020. Finally, we find a highly significant 18% increase in hours worked in the Visualisation group after nearly three years, suggesting that some participants used the workshops to develop longer-term career visions, including applying for salaried jobs.
Figure 2: Effects
Mechanisms – what can explain these effects?
We find that conventional incentivised laboratory measures of time preferences do not respond to our interventions. The interventions also have no measurable impact on self-reported planning behaviour, nor underlying cognitive functions linked to planning. In contrast, we show large, significant effects of both the Visualisation and Planning treatments on self-efficacy: both interventions strengthened participants’ belief that they can shape their own future, and overcome obstacles. After ten weeks, self-efficacy increases by 0.15 and 0.11 standard deviations, respectively. In the long-term follow-up, participants in the Visualisation group maintain significantly higher levels of self-efficacy than those in the Planning group, consistent with the differential long-term effects on chlorination.
Moreover, we find suggestive evidence of improved utility forecasting, a model of intertemporal choice recently proposed by Gabaix and Laibson (2017). Participants in the Visualisation group report significantly more clear and vivid mental forecasts of the future after almost three years. There is no such effect in the Planning group, which may explain the differential effects on both chlorination and savings. The interventions do not differentially affect beliefs and knowledge about chlorination. Summarising these findings on mechanisms, our results suggest that deeper underlying preferences and cognitive functions may not respond strongly to light-touch interventions. In contrast, beliefs about the self (such as self-efficacy) as well as the ability to imagine the future seem to be both malleable in the short and long term, and potentially powerful drivers of human behaviour.
Implications and Recommendations
Our results suggest that visualisation-based interventions might be cost-effective in increasing take-up of preventive health products and be a valuable focus of government policy. Our modules were administered by field workers with no specific training. It would thus be straightforward to incorporate them into the curricula that community health workers (CHWs) administer during household visits or community education sessions. The regularity of the work of CHWs might also overcome the fact that our effects on diarrhoea fade out after three years – effects may persist if the intervention is refreshed periodically. In the context of recent work raising concerns about the efficacy of CHW programs in improving chlorination take-up (Dupas et al 2020), our results suggest that improving the content of preventive health promotion interventions might enhance their effectiveness at a low cost.
The observed effects on savings outcomes and labour supply suggest that visualisation-based interventions might be used in other domains where policymakers wish to encourage forward-looking behaviour. Such interventions could form part of the training for members of ROSCAs or Village Savings and Loan Associations (VSLAs). They could also be used to enhance repayment discipline among borrowers of microfinance institutions.
References
Dupas, P, V Hoffmann, M Kremer, and A Peterson Zwane (2016), “Targeting Health Subsidies through a Nonprice Mechanism: A Randomized Controlled Trial in Kenya.” Science 353(6302): 889–895.
Dupas, P, B Nhlema, Z Wagner, A Wolf, and E Wroe (2020), “Expanding Access to CleanWater for the Rural Poor: Experimental Evidence from Malawi.” NBER Working Paper No. 27570.
Gabaix, X, and D Laibson (2017), “Myopia and Discounting.” NBER Working Paper No. 23254.
John, A, and K Orkin (2022), "Can Simple Psychological Interventions Increase Preventive Health Investment?", Journal of the European Economic Association 20(3): 1001-1047.
Luoto, J, D Levine, J Albert, and S Luby (2014), “Nudging to Use: Achieving Safe Water Behaviors in Kenya and Bangladesh.” Journal of Development Economics 110:13–21.
Null, C, C Stewart, A Pickering, H Dentz, N Arnold, C Arnold, J Benjamin-Chung, T Clasen, K Dewey, L Fernald, et al. (2018), “Effects of Water Quality, Sanitation, Handwashing, and Nutritional Interventions on Diarrhoea and Child Growth in Rural Kenya: A Cluster-Randomised Controlled Trial.” The Lancet Global Health 6(3): e316–e329.


