
Evidence from Iraq demonstrates that exposure to violence before birth, and the associated stress experienced by mothers, is linked to significant developmental challenges for children, shedding light on similar issues faced in other conflict zones.
The consequences of prolonged conflict extend far beyond immediate destruction and displacement. There is a profoundly impactful but less visible consequence of conflict: the long-term health effects on children who were exposed to violence in-utero. The ramifications of prenatal events for children persist well into adulthood and result in poorer mental health, educational attainment and labour market outcomes (Almond and Currie 2011, Almond et al. 2018). My research (Sardoschau 2024) focuses on the role of stress for mothers and examines how prenatal exposure to violent incidents—particularly those involving direct threats to personal safety—affects children's physical and cognitive development.
Context and data
In 2003, the United States, in conjunction with a coalition of international allies, embarked on a military campaign to oust the regime of Saddam Hussein. The initial invasion was marked by the swift collapse of the Iraqi military and the fall of the Hussein regime, culminating in the capture of Baghdad within just a few days. However, the post-invasion period was plagued by a prolonged and violent insurgency.
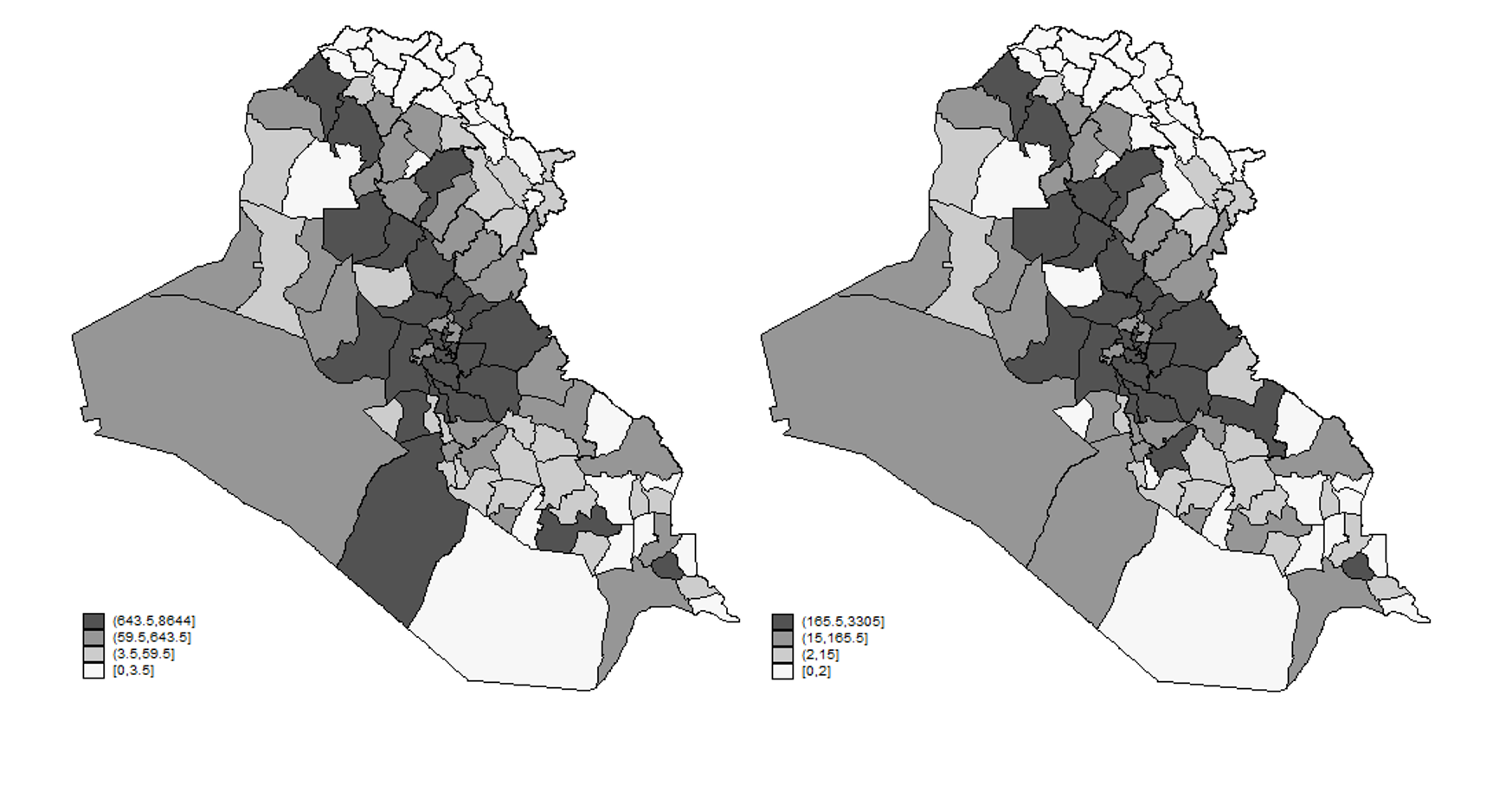
Continuous confrontations and acts of violence between coalition forces, insurgents, and sectarians have caused a total of 200,000 civilian non-combatant casualties since 2003 (Condra and Shapiro 2012, Sloboda et al. 2013). In fact, with the exception of a few Kurdish districts - all households experience at least one violent incident throughout the observation period between 2006 and 2009 (see Figure 1). According to the 2007 Iraq Mental Health Survey, 20% of female respondents reported symptoms of severe mental disorder and 5% show symptoms of post-traumatic stress disorder (PTSD). Health professionals propose PTSD as one of the main drivers through which parents transmit adverse effects to their children during war-times (Devakumar et al. 2014, Murthy and Lakshminarayana 2006).
Using detailed household data on over 36,000 children from the Multiple Indicator Cluster Survey (MICS), and geo-coded information about civilian casualties from the Iraq Body Count Project (IBC), I investigate the health outcomes of children born during and after the US invasion of Iraq between 2003 and 2009. I link information on the date, location, type, severity and perpetrator of violence to the intrauterine period of children. This detailed data allows for a comparison of health outcomes between children in the same household and with a small age gap. In essence, the empirical analysis compares the “health gap” between siblings where one has been exposed to violence in-utero to pairs of siblings where neither had been exposed to violence.
Figure 1: Cumulative number of civilian casualties (left) and violent incident (right) across districts between 2003 and 2009 (own calculations based on the Iraq Body Count Project).
A troubling legacy
The findings reveal that even a single incident of violence during pregnancy – even those with minimal impact on infrastructure (i.e. those violent incidents that cause one civilian casualty through direct gunshots, rather than explosions, missiles or bombs) – reduce a child's height and weight by 0.13 standard deviations, which translates into 370 grams and 2.7 cm for a one-year old child. In addition, children exhibit delayed cognitive development and motor skills.
Importantly, these estimates are based on “low impact” violent incidents, i.e. those with one civilian casualty, in a context where severe and prolonged episodes of violence have remained persistently high over the last 15 years. The magnitudes are therefore particularly striking since they capture the marginal effect of an additional violent incident in-utero.
Stress and access to prenatal care
These results also shed light on the varying effects of different types of violence. Incidents with a low number of casualties but a large psychological impact on the civilian population can be detrimental for child health (see Figure 2) – for example, incidents involving a public display of violence have pronounced adverse effects on children’s health. This is particularly true for sectarian violence that explicitly targets the civilian population and is religiously motivated. Violence that involves the execution and torture of civilians also has significant impacts.
While the disruption of healthcare infrastructure undoubtedly affects prenatal care, this study underscores that the stress induced by a violent environment can be equally, if not more, detrimental to prenatal development. The biological responses to stress, such as increased cortisol levels, can constrict uterine arteries and significantly reduce blood flow to the fetus. This reduction not only leads to lower birth weights and smaller sizes at birth but also predisposes children to a range of long-term issues, from decreased cognitive abilities to increased susceptibility to chronic diseases.
Figure 2: Effect of one violent incident with one civilian casualty during first trimester of pregnancy on the height for age Z-score of children, distinguishing between perpetrator and type of violence.
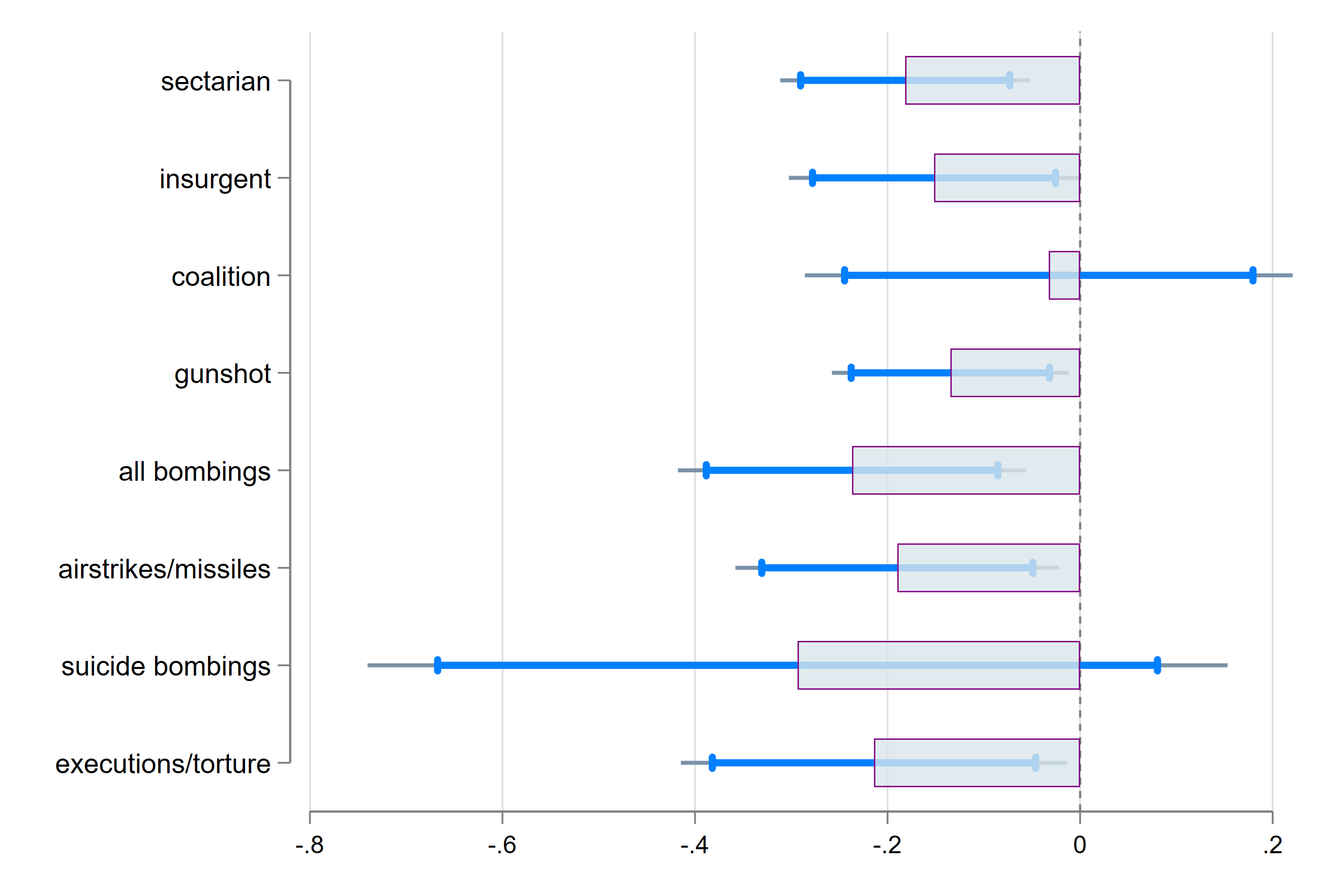
Note: Coefficient plot of dummy variable for violent incident in the district during first trimester of pregnancy, distinguishing between the perpetrator and type of violence. Separate regressions for each, dropping from the sample mothers treated by any other perpetrator/type of violence. Categories are not mutually exclusive. The dependent variable is the height for age Z-score measured by the enumerator at the time of the interview in 2011. The sample of violent incidents is restricted to “low impact” incident, i.e. those with one casualty. Control variables at the child level include gender, child birth order and a dummy variable for twins. Estimation also include year of birth dummy variables multiplied with district fixed effects, as well as mother fixed effects. Standard errors are clustered at the district level. Bars indicate point estimates. Spiked blue lines indicate 95% confidence intervals, gray lines indicate 90% confidence interval.
Against the backdrop of the large literature on the long-run effects of adverse health outcomes of children (e.g. Mansour and Rees 2012), these results highlight the importance of policies and interventions that target pregnant women particularly in places where ethnic tensions are high. The findings from this research underscore the urgent need for interventions targeted at pregnant women in conflict zones. To mitigate the effects of stress, strategies might include enhanced prenatal care, mental health counseling, and robust community support systems designed to shield expectant mothers from the harsh realities of conflict.
As regions like Iraq, Ukraine, Gaza and others grapple with years of conflict, understanding the full scope of war's impact, including its effects on unborn children, is crucial. This study serves as a stark reminder that the costs of conflict extend far into the future, affecting even those not yet born when the fighting occurred. For a healthier, more stable future, interventions that protect and support the most vulnerable, particularly pregnant women and their unborn children, are essential amidst war and conflict.
References
Almond, D and J Currie (2011), "Killing me softly: The fetal origins hypothesis", Journal of Economic Perspectives, 25(3): 153–72.
Almond, D, J Currie, and V Duque (2018), "Childhood circumstances and adult outcomes: Act II", Journal of Economic Literature, 56(4): 1360–1446.
Condra, L N and J N Shapiro (2012), "Who takes the blame? The strategic effects of collateral damage", American Journal of Political Science, 56(1): 167–187.
Devakumar, D, M Birch, D Osrin, E Sondorp, and J C Wells (2014), "The intergenerational effects of war on the health of children", BMC Medicine, 12(1): 57.
Mansour, H and D I Rees (2012), "Armed conflict and birth weight: evidence from the Al-Aqsa Intifada", Journal of Development Economics, 99(1): 190–199.
Murthy, R S and R Lakshminarayana (2006), "Mental health consequences of war: a brief review of research findings", World Psychiatry, 5(1): 25–30.
Sardoschau, S (2024), "In utero exposure to violence and child health in Iraq", Journal of Population Economics, 37(2): 40.
Sloboda, J, H Dardagan, M Spagat, and M H R Hicks (2013), "Iraq Body Count: A case study in the uses of incident-based conflict casualty data", in Seybolt, Aronson, and Fischhoff, Counting Civilian Casualties, 53.

