
Poverty, low social capital and low government administrative capacity hinder sanitation improvements, even when the health benefits are clear.
It is estimated that around 500 million people worldwide practice open defecation as a result of inadequate access to sanitation facilities, leading to a tremendous disease and mortality burden that most severely impacts children and the poor (WHO/UNICEF 2021).
Proper sanitation reduces the spread of illnesses such as diarrhoea and typhoid, which can be transmitted through faecal matter. In countries where people practice open defecation in rivers, fields and forests, these illnesses are harder to stop. Faecal matter is tracked into homes and into food, causing life-threatening disease, particularly among infants and children under the age of five.
Development practitioners and policymakers seeking to improve sanitation and reduce open defecation are still searching for the most effective programmes. Financial constraints, inadequate water systems and behavioural habits all play a role in slowing the end of open defecation.
One proposed solution to discourage open defecation is Community Led Total Sanitation (CLTS). CLTS is a community-led approach that seeks to engage community members to create demand for sanitation and produce “open defecation free” communities. In our paper we evaluate the effectiveness of Community-Led Total Sanitation (CLTS) at scale in Indonesia via a randomised trial to see whether it can improve sanitation and child health (Cameron et al. 2019).
What is CLTS?
CLTS involves facilitators initiating a community analysis of existing sanitation practices, highlighting the negative health consequences that flow from poor sanitation. In essence, it involves telling participants that faecal contamination spreads from exposed excreta to living environments, food and drinking water, and that everyone is ingesting small amounts of faecal material. In this way, CLTS aims to shame communities into improving their sanitation. The community actively participates in the facilitated meeting and is then left to forge its own plan to improve village sanitation with only limited follow-up support and monitoring from the programme.
CLTS stands in contrast to traditional sanitation programmes that take a supply-side approach by providing or subsidising sanitation hardware and infrastructure. The programme is viewed by many as the most promising sanitation intervention available–this is reflected in the fact that CLTS has been implemented in over 60 countries worldwide by NGOs, the World Bank and, increasingly, governments, with many having adopted CLTS as national policy (Zuin et al. 2019).
In our study, CLTS was implemented by resource agencies hired by the World Bank’s Water and Sanitation Programme in approximately half the treatment communities, and resource agency-trained local government officials in the remaining locations.
Data collection and evaluation design
We drew on data from around 2000 households across 160 rural communities in eight districts in East Java, Indonesia. Households were first interviewed in August/September 2008 (just prior to programme implementation) and again approximately 24 months later between November 2010 and February 2011. Half of these communities were randomly assigned to receive CLTS, with the other half receiving no sanitation intervention.
Since CLTS seeks to promote sanitation, improve health (especially among children), and stimulate attitudinal change, we focused on these outcomes in our evaluation. We collected information from respondent households on their attitudes to open defecation and sanitation. We measured and weighed children under 2 years of age at baseline and again approximately two years later at endline so we could examine impacts on growth. Blood and faecal samples were also collected from children to allow tests for anaemia and worm infestations.
The impacts of the CTLS programme
The CLTS programme had positive impacts on a range of sanitation and health outcomes. We found that CLTS increased the rate of toilet construction by about 19%, decreased community tolerance of open defecation, and reduced the prevalence of roundworm infestations among children by around 46%. However, no effects were found on child anaemia or child growth.
Poorer households could not afford to build toilets
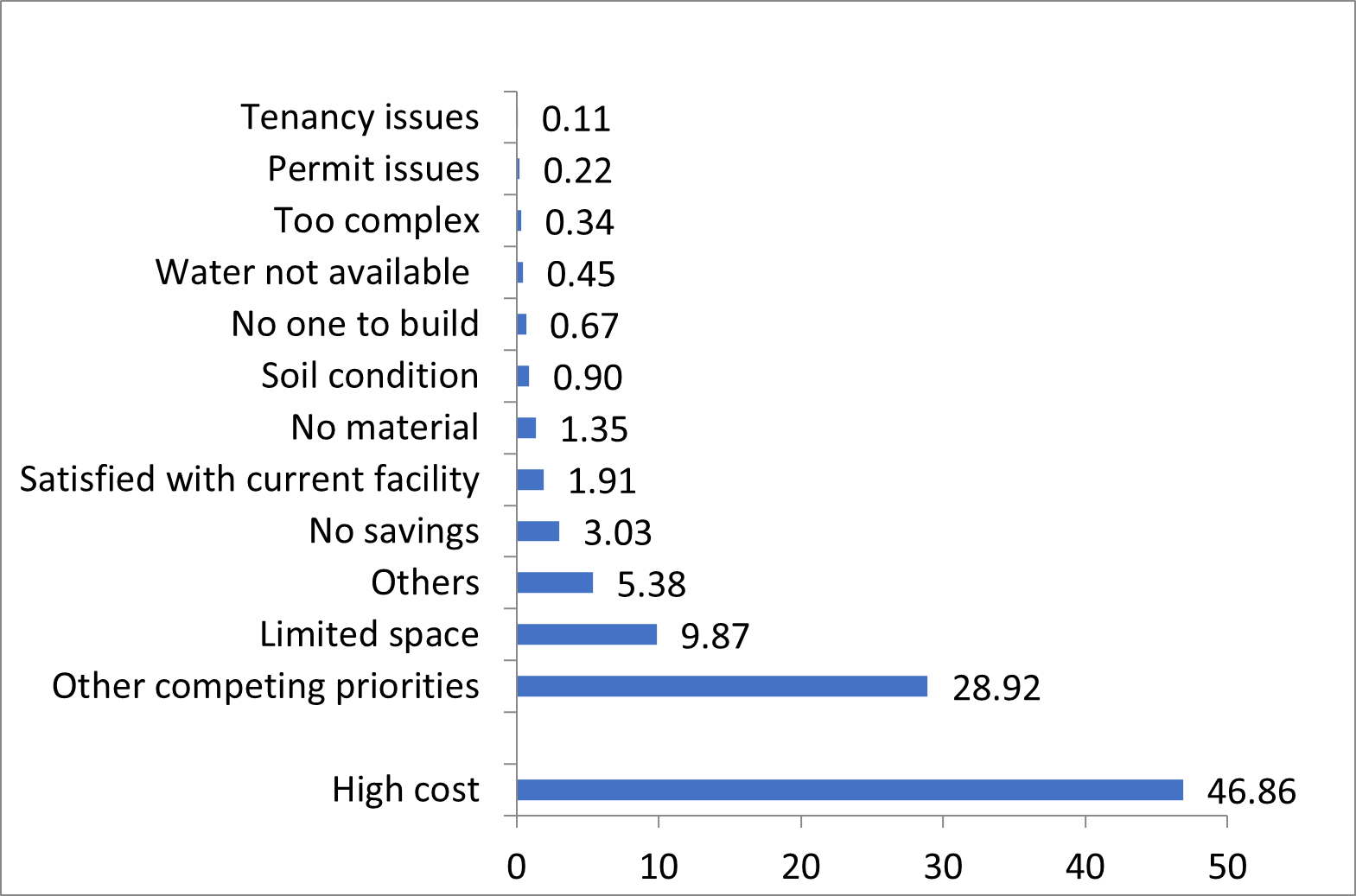
The benefits of the programme were not spread uniformly across all participants as poorer households were unable to afford to build toilets. As Figure 1 shows, cost was the most frequently reported obstacle to building a toilet (reported to be an obstacle by 47% of households) and toilet construction did not increase among the poorest households. This calls into doubt the CLTS ethos of no subsidies (see Kar and Pasteur 2005) and suggests that financial assistance of some sort to enable poorer households more fully participate is likely warranted.
Figure 1: Main reason for not building a toilet
Further research by one of the authors in Laos does indeed find that the provision of partial rebates to poorer households on completion of toilet construction is effective in encouraging poorer households to participate (Cameron et al. 2021). In the Laos setting, community-wide incentives that were hoped to incentivise community members to assist poorer households did not increase the probability of poorer households installing sanitation.
Private sector agency provision was more effective than government implementation
Variation in impact was not just driven by household poverty levels, but which agents implemented the programme in a particular area. In fact, the positive impacts on toilet construction and child health were almost entirely driven by villages who received CLTS implemented by private sector agencies who were contracted by the World Bank. In the other implementation areas, where the private sector agencies had trained local government officials in CLTS implementation and then handed the project over to government, no discernible benefits were produced. This was attempted as government engagement was deemed crucial in the ability to get the CLTS programme rolled out at scale and for local ownership of the programme. Unfortunately, analysis shows that local government implementers typically engaged less with village staff, made fewer community visits and achieved lower levels of community participation.
Communities with low social capital did not respond well to the shaming aspect of CLTS.
The programme also had perverse effects in communities with low levels of social capital. This is because communities with a greater degree of pre-existing community interaction are likely to be better prepared to cooperate and have a greater store of community knowledge on which to draw when targeting the poor and prioritising community needs (Chambers 2009). Conversely, communities with low stocks of social capital might struggle to work together and agree on community priorities.
Our analysis shows that low social capital communities were less able to successfully impose social sanctions on non-compliers, reducing the effectiveness of the shaming that is part of CLTS. As a result, toilet construction suffered and health benefits were less likely to be realised.
What does this mean for policy?
Our findings demonstrate the potential for CLTS to improve sanitation and child health outcomes, while highlighting that generating demand for sanitation does not overcome the affordability challenges faced by poorer households. Without assistance many poor households are unable to afford to improve their sanitation, no matter how much they may desire to. Thus, one danger of CLTS is that the shaming which is its driving force may land disproportionately on the most disadvantaged. The CLTS strategy of not providing financial assistance to the poor hence warrants attention.
Moreover, the study demonstrates that in order to scale the programme up effectively, investing in implementation capacity is essential. Greater resourcing is needed, particularly in low social capital communities where building of relationships with the local community is necessary for community buy-in.
References
Cameron, L, S Olivia and M Shah (2019), “Scaling up sanitation: Evidence from an RCT in Indonesia”, Journal of Development Economics, 138:1-16.
Cameron, L, P Santos, M Thomas and J Albert (2021), “Sanitation, financial incentives and health spillovers: A Cluster Randomised trial”, Journal of Health Economics, 77:102456
Chambers, R (2009), “Going to Scale with Community-led Total Sanitation: Reflections on Experience, Issues and Ways Forward”, IDS Practice Paper, 1:1-4
Kar, K, K Pasteur (2005), “Subsidy or Self-respect? Community Led Total Sanitation. An Update on Recent Developments”, IDS Working Paper, 257.
WHO/UNICEF (2021), “Progress on household drinking water, sanitation and hygiene 2000 - 2020: Five years into the SDGs.”
Zuin, V, C Delaire, R Peletz, A Cock-Esteb, R Khush and J Albert (2019), “Policy diffusion in the rural sanitation sector: lessons from community-led total sanitation(CLTS)”, World Development, 124:104643



