
The offer of an appointment more than doubled the likelihood of men getting an HIV test, and was most effective for men wanting a commitment device
It is easy to put off healthcare, and especially preventive care. Doctor visits take time, procedures can involve pain or discomfort, and routine tests cause anxiety (Oster et al. 2013). For the most part, these inconveniences are offset by the long-run benefits of an early diagnosis, but procrastination is a problem (DellaVigna and Malmendier 2006). Behavioural economics suggests an elegant solution: allow people to voluntarily commit to healthcare by putting money down as collateral. This type of contract with one’s self is called a commitment device or commitment contract, and has been shown to help people overcome many types of self-control problems, from quitting smoking (Gine et al. 2010) and drinking (Schilbach 2019), to getting people to go to the gym (Royer et al. 2015).
Bai et al. (2020) show that when it comes to attending doctor visits, people want a commitment device. They offer various types of commitment contracts to hypertensive patients in India and find take-up rates of between 14% and 39%. However, these contracts can backfire – most people in their study do not follow through on the commitment and lose the money. This demonstrates a key problem with commitment devices: they only work if people are sufficiently sophisticated, i.e. they are aware of their self-control problems. If a person underestimates just how bad their tendency to procrastinate is, they might sign a contract that, when it comes down to it, is not strong enough to make them follow through. Bai and co-authors therefore, show that offering people a completely voluntary commitment contract can make the average person worse off.
Healthcare appointments as a tool for overcoming commitment problems in Malawi
In recent research (Derksen, Kerwin, Ordaz Reynoso, and Sterck 2021), we find evidence in favour of a simple, more effective alternative: healthcare appointments. Appointments are typically used in healthcare to increase efficiency at clinics and hospitals (Steenland et al. 2019), but they also operate as a natural bundle of behavioural interventions, or nudges. These nudges, which include prompting people to make a concrete plan, offering default options, or sending reminders, are often moderately effective on their own (e.g. Milkman et al. 2011). When combined, they can have a large impact on healthcare demand (Salvadori et al. 2020).
In Malawi, a country in southern Africa, HIV prevalence is around 10%, but the HIV testing rate is low, especially for men. While HIV treatment saves lives and prevents transmission, early diagnosis is key. Since routine testing and treatment are offered during prenatal care, men are less likely to get HIV treatment and are more likely to die of AIDS (Dovel et al. 2015). We examine the effect of offering appointments on HIV testing decisions using a sample of 1,200 high-risk men in Malawi. We find that most men do want to get tested for HIV, but have self-control problems; half the men in our sample demand a financial commitment device for HIV testing. We show that men who are randomly assigned to actually receive such a commitment device are more likely to get an HIV test; however, over half of the people who get a commitment device do not follow through, and thus, end up losing their collateral.
Figure 1 HIV testing rates by study arm
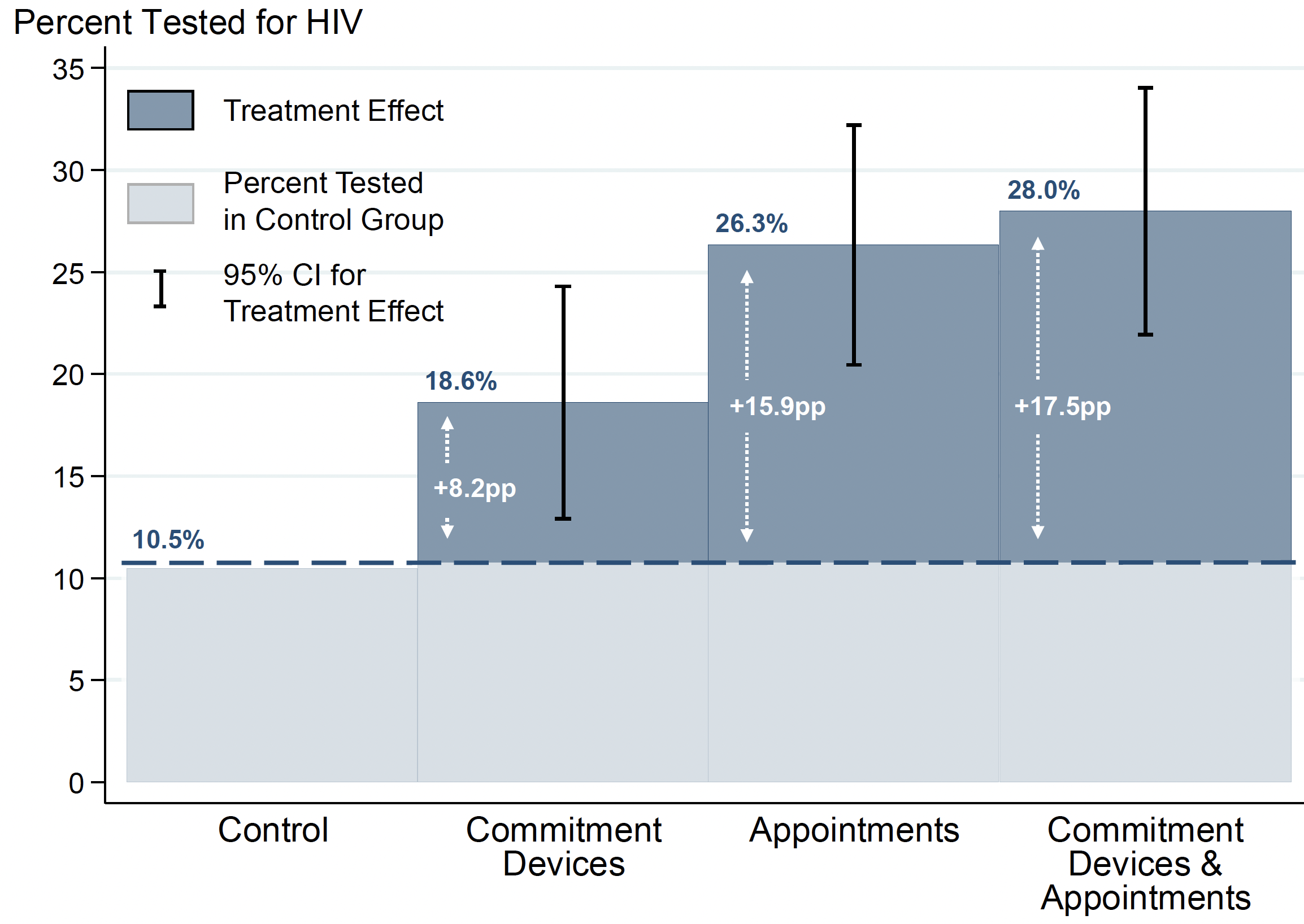
Note: Bars represent fitted values for the HIV testing rate in each study arm, based on a linear regression with pre-specified control variables. Whiskers show 95 percent confidence intervals for the differences between the control group and each treatment group. We can reject the that the appointments group and the control group have equal testing rates, and also that the appointments treatment and the commitment devices treatment have equal testing rates.
In contrast, we find that appointments are much more effective. Men who were randomly assigned to be offered an appointment increased their HIV testing rate by over 100% compared with the control group – an effect twice as large as that of commitment devices. Appointments work especially well for the men who demand commitment, and dominate commitment devices overall. Indeed, offering a commitment device on top of an appointment carries close to zero additional benefit.
Figure 2 Spike in testing on appointment date
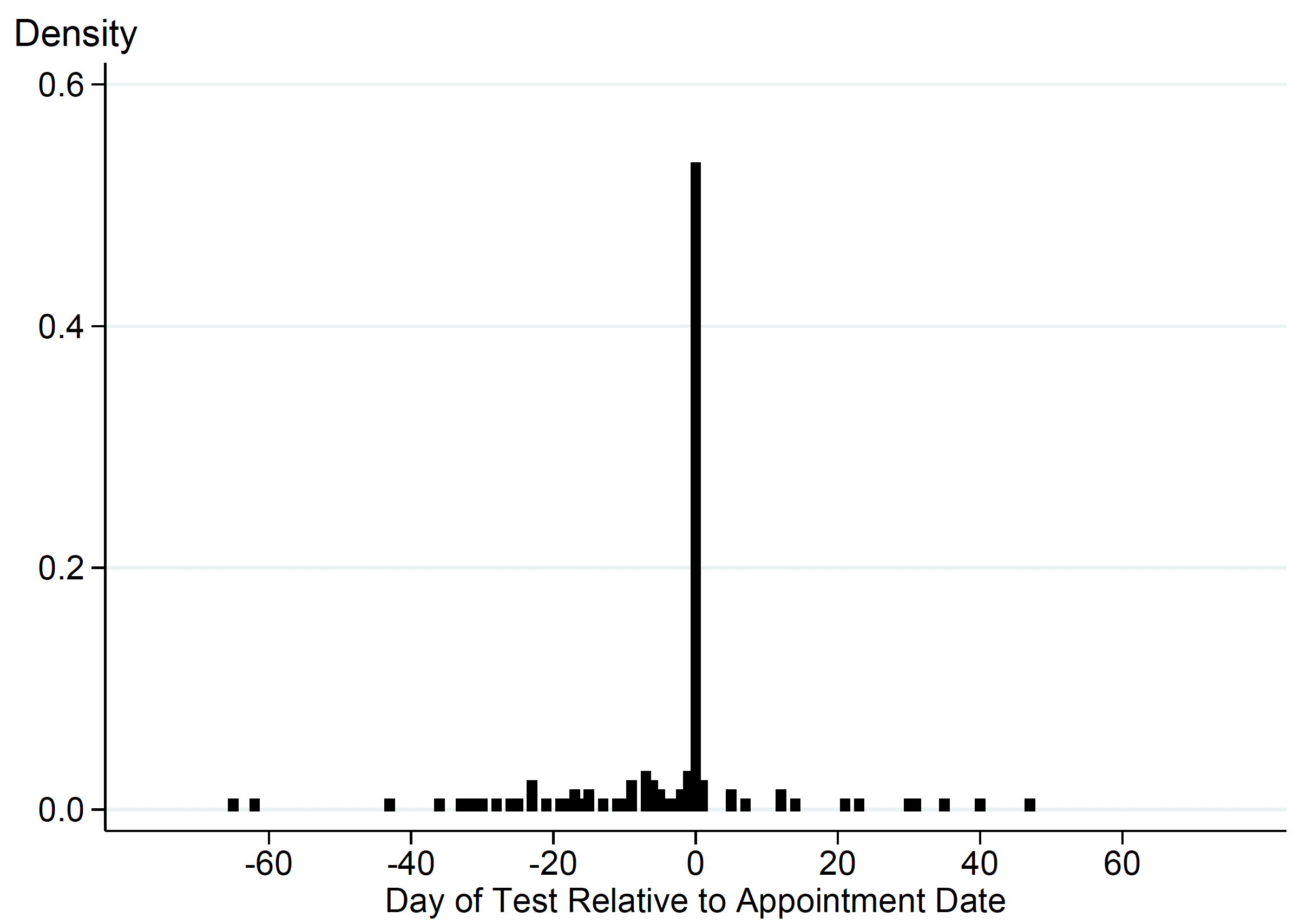
Note: Histogram of HIV test timing relative to appointment date (using the new date for men who rescheduled their appointments). Appointment is at day 0; there is a large spike in testing on the date of the appointment.
Why are appointments more effective than traditional commitment devices?
It seems that appointments operate as social commitment devices. Just knowing that a clinician is waiting might help a person to stop procrastinating and get the test. We do see a large spike in testing on the actual date of the appointment as opposed to on other dates, which could be due to the pressure to show up for a waiting clinician. However, the social commitment aspect is likely not the only channel through which appointments increase the demand for HIV tests. Having an appointment may make men feel welcomed at the clinic, which might be important (Dovel et al. 2020). In addition, the reminders that come with appointments likely work on people who are prone to forgetting their plans. Indeed, we see that people in the appointments group are more likely to get tested later in the study window, even outside of the appointment date. Another potential channel is shorter wait times, but qualitative data suggests that there is usually little to no wait for an HIV test in our context. Finally, appointments make a particular date salient, and prompt people to make a concrete plan; although, at least for HIV testing, planning prompts have been found ineffective on their own (Macis et al. 2021). Health appointments combine all of these features, with the whole seeming to be greater than the sum of the parts.
Figure 3 Test dates for those who test outside of appointment date
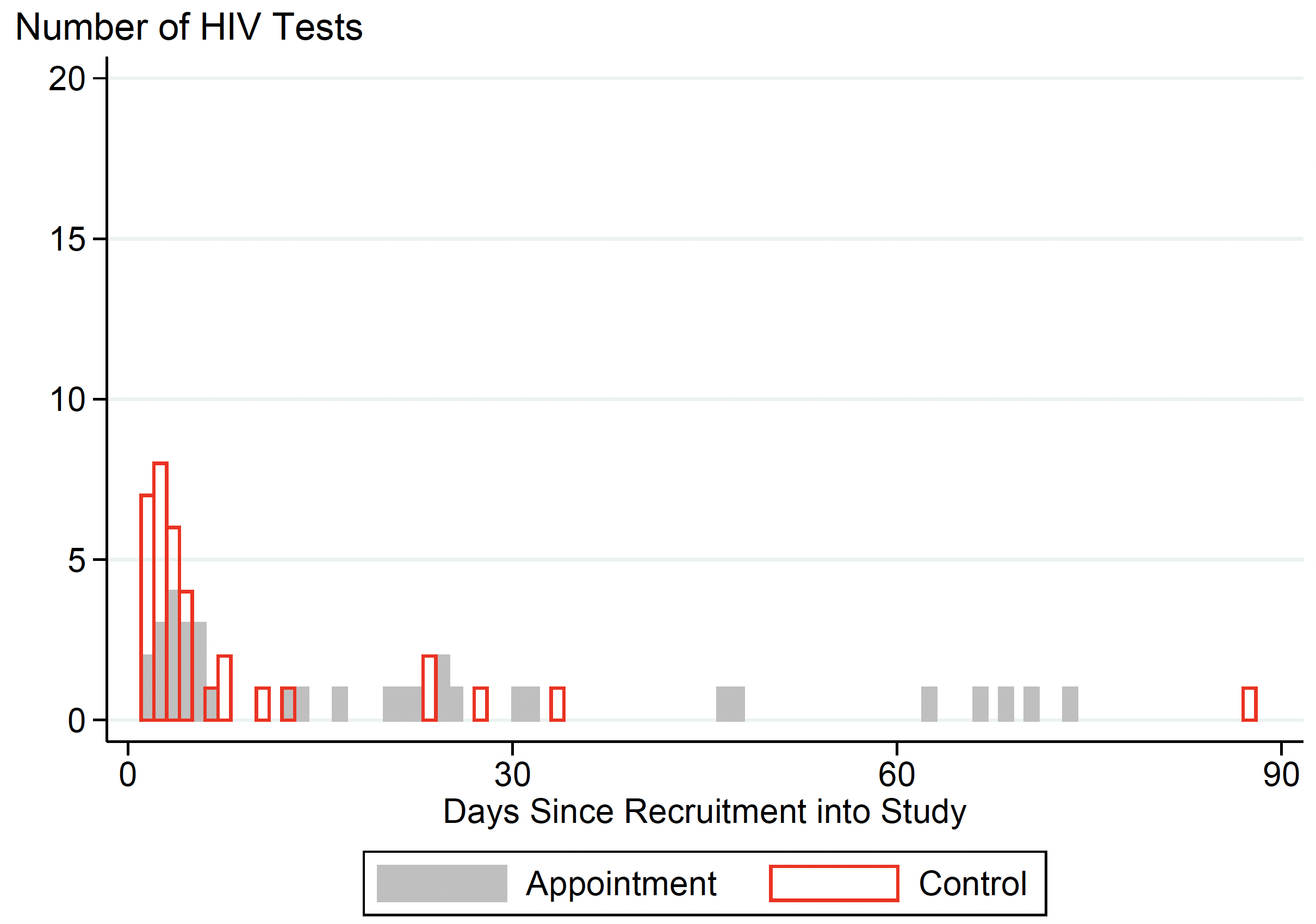
Note: Histogram of HIV test timing relative to the date the subject was recruited, i.e. the baseline survey date. Recruitment is at day 0. Sample includes all control-group men who got an HIV test and men from the pure appointments group who got an HIV test outside of their appointment date. There is far more testing late in the study period in the appointments group that in the control group.
Appointments, like other commitment devices, are voluntary rather than coercive. They are likely to work well for healthcare services that people generally desire but tend to put off, such as routine tests and check-ups, flu shots, and COVID-19 booster shots. An appointment is unlikely to change the behaviour of a person who is genuinely opposed to care. Indeed, Chang et al. (2021) find that sending a link to an appointment scheduler has no impact on COVID-19 vaccination amongst vaccine-hesitant people in California.
Overcoming efficiency problems and long-run costs from delayed care
Our findings are especially relevant for poor countries, where the health burden is severe and yet, most routine care is offered on a walk-in basis. In order to schedule appointments and issue reminders, clinics need access to technology, and an ability to communicate with patients. The recent rise in mobile phone ownership, as well as internet access, have made appointments feasible where they once were not.
Appointments lead to obvious efficiency gains for clinics and hospitals, and for this reason, are nearly universally required in developed-country healthcare settings. They also act as a surprisingly effective behavioural tool. They are more effective than commitment devices, including and especially amongst people with self-control problems. Appointments should be attractive to clinics and hospitals amongst many dimensions, and relatively straightforward to implement. Commitment devices, like incentives, are more complicated, because they involve money. To use them, clinics would have to collect or withhold money from patients. Moreover, because many patients sign up for a commitment device but do not follow through, offering a commitment device can actually make many or even most patients worse off.
By introducing scheduled health appointments for routine care, poor countries can address efficiency problems and healthcare demand problems at the same time. Most importantly, they can mitigate the long-run health and economic costs that arise from delayed care. In the case of the HIV epidemic, which is now concentrated in poor countries, appointments can mean earlier diagnoses, earlier treatment, fewer new infections, and fewer unnecessary deaths.
References
Bai, L, B Handel, E Miguel and G Rao (2017), “Self-control and demand for preventive health: Evidence from hypertension in India”, The Review of Economics and Statistics, 1-55.
Chang, T, M Jacobson, M Shah, R Pramanik and S B Shah (2021), “Financial Incentives and Other Nudges Do Not Increase COVID-19 Vaccinations among the Vaccine Hesitant”, NBER Working Paper No. w29403).
Chapman, G B, M Li, H Leventhal and E A Leventhal (2016), “Default clinic appointments promote influenza vaccination uptake without a displacement effect”, Behavioral Science & Policy 2(2): 40-50.
DellaVigna, S and U Malmendier (2006), “Paying not to go to the gym”, American Economic Review 96(3): 694-719.
Derksen, L, J Kerwin, N O Reynoso and O Sterck (2021), “Appointments: A More Effective Commitment Device for Health Behaviors”, Working Paper.
Dovel, K, S L Dworkin, M Cornell, T J Coates and S Yeatman (2020), “Gendered health institutions: examining the organization of health services and men’s use of HIV testing in Malawi”, Journal of the International AIDS Society 23; e25517.
Dovel, K, S Yeatman, S Watkins and M Poulin (2015), “Men’s heightened risk of AIDS-related death: the legacy of gendered HIV testing and treatment strategies”, AIDS 29(10): 1123.
Giné, X, D Karlan and J Zinman (2010), “Put your money where your butt is: a commitment contract for smoking cessation”, American Economic Journal: Applied Economics 2(4): 213-35.
Macis, M, M Grunauer, E Gutierrez, R Izurieta, P Phan, M R Ortiz, M. R., ... and E Teran (2021), “Using Incentives and Nudging to Improve Non-Targeted HIV Testing in Ecuador: A Randomized Trial”, AIDS and Behavior, 1-9.
Milkman, K L, J Beshears, J J Choi, D Laibson and B C Madrian (2011), “Using implementation intentions prompts to enhance influenza vaccination rates”, Proceedings of the National Academy of Sciences 108(26): 10415-10420.
Oster, E, I Shoulson and E Dorsey (2013), “Optimal expectations and limited medical testing: evidence from Huntington disease”, American Economic Review 103(2): 804-30.
Royer, H, M Stehr and J Sydnor (2015), “Incentives, commitments, and habit formation in exercise: evidence from a field experiment with workers at a fortune-500 company”, American Economic Journal: Applied Economics 7(3): 51-84.
Salvadori, N, P Adam, J Y Mary, L Decker, L Sabin, S Chevret, ... and G Jourdain (2020), “Appointment reminders to increase uptake of HIV retesting by at‐risk individuals: a randomized controlled study in Thailand”, Journal of the International AIDS Society 23(4): e25478.
Schilbach, F (2019), “Alcohol and self-control: A field experiment in India”, American Economic Review 109(4): 1290-1322.
Steenland, M, J Dula, A De Albuquerque, Q Fernandes, R M Cuco, S Chicumbe, ... and M McConnell (2019), “Effects of appointment scheduling on waiting time and utilisation of antenatal care in Mozambique”, BMJ Global Health 4(6): e001788.




