
Providing small financial incentives for daily steps to at-risk individuals in India encouraged exercise and improved health
Lifestyle diseases like diabetes and hypertension are growing problems around the world with both economic and human costs. Currently 537 million adults are living with diabetes with that number expected to rise to 643 million by 2030 (IDF Diabetes Atlas). While diabetes is a global challenge, low- and middle-income countries carry a heavy burden - over three in four adults with diabetes live in these countries (IDF Diabetes Atlas). In 2021, the global direct costs of diabetes were US$ 966 billion, and the disease caused 6.7 million deaths (IDF Diabetes Atlas).
Lifestyle changes like increasing physical activity or eating a healthier diet can prevent diabetes and the various long-term complications associated with the disease. However, these behaviour changes, like many others, can be hard for individuals to take up and adhere to as they may have immediate time and effort costs while benefits may not be realised until much later. This presents a challenge because impatient individuals, who undervalue the future relative to the present, may postpone necessary lifestyle modifications. Of the existing evidence-based lifestyle change interventions, many are costly and intensive to implement (Howells et al. 2016). Could incentives, which are increasingly common in behaviour change programmes, help encourage impatient individuals to adopt healthy behaviours now and curb procrastination?
In our recent paper (Aggarwal, Dizon-Ross, and Zucker 2022), we partnered with the Government of Tamil Nadu, which is interested in scalable interventions to promote lifestyle changes among diabetics, to study this question in the southern Indian city of Coimbatore. India is facing a diabetes epidemic and it accounts for one in seven of all adults living with diabetes worldwide. It also has the second largest number of adults with undiagnosed diabetes at 39.4 million people as of 2021 (IDF Diabetes Atlas). Additionally, nearly US$ 8.5 billion was spent on diabetes in India in 2021 alone (Diabetes Data Portal).
Experimental design: Incentivising behaviour change
Our programme monitored participants’ walking using pedometers and, if they achieved a daily step target of 10,000 steps, provided them with a small financial incentive paid out in mobile phone credits. Via public screening camps we identified a sample of nearly 3,200 individuals with diabetes or high blood sugar, a risk factor for diabetes, and randomly assigned participants to one of eight groups for twelve weeks:
- Incentives Groups: Individuals received pedometers to monitor their daily step total and incentives for walking at least 10,000 steps a day. Six different types of incentive contracts were evaluated which varied the amount and frequency of payment as well as the minimum number of days per week that the step target had to be met.
- Monitoring group: Individuals received only pedometers and were encouraged to wear them and report their steps every day.
- Comparison group: Individuals received neither pedometers nor incentives.
Participants in both the incentives and monitoring groups reported their steps daily to an automated calling system. We visited participants three times over the course of the twelve-week programme to sync pedometers, verify self-reported steps, and collect biometric and mobile phone usage data. We also conducted a baseline health survey that included health measures such as HbA1c (a measure of blood sugar control and the most common measure of diabetes risk), body mass index (BMI), blood pressure, and mental health. In addition, we collected baseline walking data, assessed participants’ impatience through questions on preferences, and conducted an endline survey to gather health, fitness, and lifestyle information.
Experimental evidence
Overall, incentivising walking led participants to walk more while also reducing risk factors for diabetes and mental health. Furthermore, among impatient individuals, incentives with a minimum threshold of days walked were effective and may also be more cost-effective.
Incentives were effective at encouraging exercise
Providing INR20 (US$ 0.33) per day of reaching the step target increased compliance by 20 percentage points (a 67% increase) relative to the monitoring group (Figure 1). Individuals did not just shift steps from one day to another–incentives increased walking by 1,266 steps per day (a 20% increase) or approximately thirteen minutes of brisk walking. This is among the higher effect sizes found in other adult populations (Bachireddy et al. 2019, Finkelstein et al. 2016). Steps also increased among those who did not meet their daily target and the incentives’ impact on walking remained stable throughout the programme’s duration.
Figure 1: Incentives increase average walking
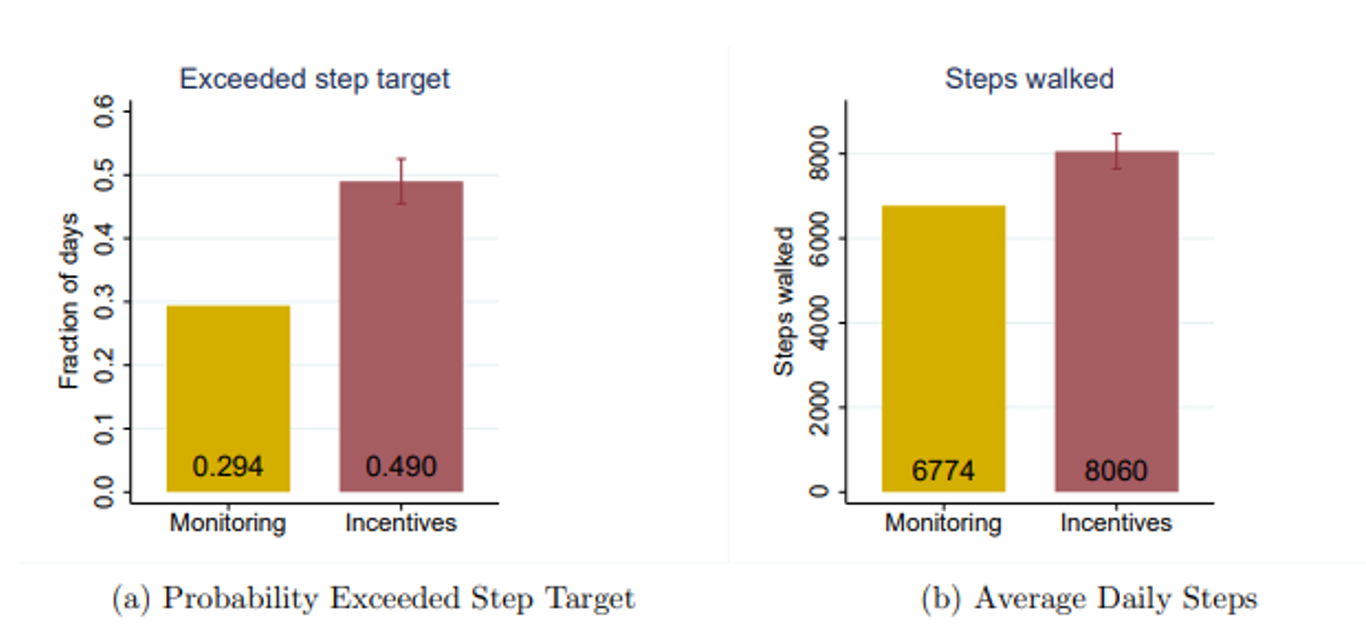
Notes: The figure displays the impact of the pooled incentive treatments on walking during the programme. Panel A shows the average probability of exceeding the daily 10,000 step target; Panel B shows average daily steps walked.
Incentives’ impact on walking sustained: Individuals in the incentive groups continued to walk more than the monitoring group even after incentives were no longer provided, although this was only 60% as much as they did during the programme. This impact persisted twelve weeks after the incentives ended, suggesting that short-term incentives may help individuals form lasting habits and be cost-effective.
Incentives moderately improved physical and mental health: Health outcomes, measured by an index of five health risk factors, improved by 0.05 standard deviations among the incentive groups relative to the comparison group. Incentives also led to a 0.09 standard deviation improvement on a mental health index with participants reporting feeling happier and less worn. The positive effect on mental health may be from increased exercise, the financial reward, or a combination of the two.
Threshold contracts were more effective for impatient individuals: For impatient participants the threshold payments increased their step target compliance by 6 percentage points as compared to patient individuals (Figure 2). In contrast, threshold payments decreased patient individuals’ step completion by 3.4 percentage points relatives to individuals who did not receive threshold payments. Additionally, variance in compliance was significantly higher in the threshold group than the base incentive group—thresholds caused significantly more people to meet the target on either zero or seven days. These results highlight an important consideration for policymakers —incentives should be targeted or tailored to the patience of the individual.
Figure 2: Threshold payments increase walking more for impatient individuals
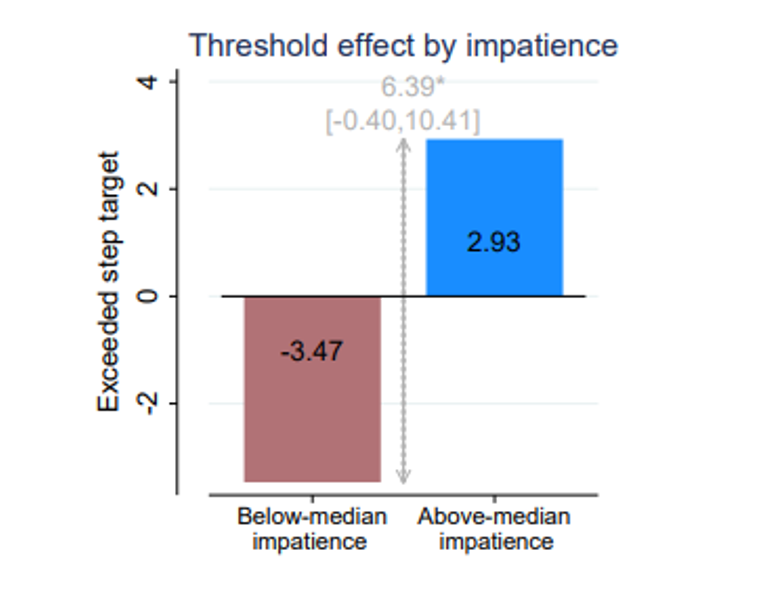
Notes: This chart plots the effect of the threshold contract relative to the base payment, estimated separately for those with below-median predicted impatience (left bar) versus above-median predicted impatience (right bar). The height of the vertical arrow shows the difference between the treatment effects, with the 95% confidence interval in brackets.
Increasing payment frequency had no effect on steps walked: Differing from common belief, more frequent payment—in this case daily—was no more effective at increasing steps than the weekly or monthly payment schedules. This suggests that while impatience in the effort domain is important for incentive design, impatience in the reward domain may be less so. Furthermore, walking behaviour remained steady across the weekly and monthly payment cycles, not increasing as payday approached which would have been expected if individuals were impatient over payments.
Threshold incentive contracts were the most-cost effective: Individuals in the four-day and five-day threshold incentive groups did not always meet their target on the requisite number of days per week and were therefore respectively paid an average of 10 to 15% less than the amount paid through other contract options while generating the same amount of walking. The cost-effectiveness of these contracts were 11% and 17% higher than that of the base incentive contract.
Policy implications and further research
Exercise has important health effects for individuals diagnosed with diabetes, but other interventions proven to improve exercise among diabetic or prediabetic populations have required highly trained staff and personalised interactions (Qiu et al. 2014, Aziz et al. 2015). Our study is the first to suggest that scalable, low-intensity, low-cost programmes can be successful at increasing exercise among diabetics. The per-person cost of the incentive programme was INR1,700 (US$ 26), which is equal to just 7% of the estimated annual direct cost of care for a diabetic in Tamil Nadu.
Additionally, the persistence of the impact on walking suggests that policymakers could extend the intervention, or make it permanent, and expect similar effects. While threshold contracts were highly effective at motivating impatient individuals, they actually decreased walking among patient individuals suggesting that policymakers should consider individualising who receives such contracts based on impatience to increase both programme effectiveness and cost-effectiveness.
We have been exploring a scale-up of the programme in partnership with the Government of Tamil Nadu and have also conducted a follow-up study on how incentive contracts can be customised to individuals based on observable characteristics or incentivise individuals to choose their preferred contract type (Dizon-Ross and Zucker 2023).
References
International Diabetes Federation (IDF) (2021), “IDF Diabetes Atlas, 10th Edition”, Available here.
Sun H, P Saeedi, S Karuranga, M Pinkepank, K Ogurtsova, B B Duncan, C Stein, A Basit, J C Chan, J C Mbanya, and J C, and M E Pavkov (2021), "IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045", Diabetes research and clinical practice, 183: 109119.
Howells, L, B Musaddaq, A J McKay, and A Majeed (2016), “Clinical impact of lifestyle interventions for the prevention of diabetes: An overview of systematic reviews”, BMJ Open 6(12): e013806.
International Diabetes Federation (IDF) (2021), “Diabetes Data Portal”, Available here.
Bachireddy, C, A Joung, L K. John, F Gino, B Tuckfield, L Foschini, and K L Milkman (2019), “Effect of different financial incentive structures on promoting physical activity among adults: A randomized controlled trial”, JAMA Network Open 2(8): e199863-e199863.
Finkelstein, E A, B A Haaland, M Bilger, A Sahasranaman, R A Sloan, E E K Nang, and K R Evenson (2016), “Effectiveness of activity trackers with and without incentives to increase physical activity (trippa): A randomised controlled trial”, The Lancet Diabetes and Endocrinology 4(12): 983–995.
Qiu, S, X Cai, U Schumann, M Velders, Z Sun, and J M Steinacker (2014), “Impact of walking on glycemic control and other cardiovascular risk factors in type 2 diabetes: A meta-analysis." PLoS one 9(10): e109767.
Aziz, Z, P Absetz, J Oldroyd, N P Pronk, and B Oldenburg (2015), “A systematic review of real-world diabetes prevention programs: Learnings from the last 15 years”, Implementation Science 10(1): 1-17.
Dizon-Ross, R and A Zucker (2023), “Mechanism Design for Personalized Policy: A Field Experiment Incentivizing Behavior Change”, Technical report, Working paper, University of Chicago.



