
There are stark gender disparities in hospital usage in India which increase with the cost of care. Social subsidies are unlikely to close disparities without gender-targeted efforts
There are an estimated 63 million missing females in India. While attention has largely focused on gender disparities at birth and early childhood, almost two-thirds of those missing are adult and elderly women, highlighting the important role of inputs throughout the life-cycle (Anderson and Ray 2010). As the burden of non-communicable disease such as cancer, diabetes, and cardiovascular conditions has grown, accounting for one in two deaths among women in 2018 (Bhan and Shukla 2023), affordable access to hospital care is increasingly important.
Subsidising healthcare has been a key policy for reducing inequalities in access, including along gender. Over the last 15 years, India has expanded government health insurance programmes to provide free care to low-income households at public and approved private hospitals. In 2019, the central government launched the national PMJAY health insurance programme that covers the poorest 40% of the Indian population, making it the largest such programme in the world. The program,e is a key piece of the government’s efforts to achieve universal health coverage and reducing inequalities is an explicit goal. In our research (Dupas and Jain 2024), we provide evidence that large gender disparities persist within government insurance and explore why this may be the case.
We study the Bhamashah Swasthya Bima Yojana (BSBY) health insurance programme launched in Rajasthan in December 2015. The program is very similar in design to the national PMJAY programme. We compile insurance claims data on all 4.2 million hospital visits between 2016 and 2019. The claims include patient age, gender, residential address, the hospital visited, admission and discharge dates, and services received. We geocode hospital and patient residence locations, allowing us to measure the distance to hospitals and distance travelled for every hospital visit. We also link the claims to census and three rounds of village electoral (Gram Panchayat) data. This provides some of the most detailed hospitalisation data in India, allowing us to study insurance utilisation with unusual granularity.
A framework to understand gender disparities in use of social services
A simple conceptual framework can explain why gender inequalities in the use of social services, including and beyond healthcare, may persist despite large subsidies, and helps think through the likely impact of different types of policy interventions. In the presence of gender-biased societal norms and practices, household usage of services will be lower, and more sensitive to costs, for females relative to males. This implies that, if services are not costless, household will use them less for females than males and higher costs will be associated with larger gender disparities (Findings 1 and 2).
Given this, a natural assumption would be that reducing costs will reduce gender gaps. Indeed, this is part of the motivation behind subsidies in the first place. A crucial contribution of the paper is to show that this simple intuition is, in fact, not always correct. A gender-neutral subsidy increase may raise female levels of utilisation but fail to lower gender disparities if males benefit as much or more (Finding 3). In contexts of female disadvantage, gender-targeted strategies that directly address the factors lowering female usage relative to males are an important complementary strategy that can increase the effectiveness of subsidies in lowering gender gaps (Finding 4).
Finding 1: Stark gender disparities in hospital usage
We first document striking, persistent gender disparities in hospital utilisation despite the insurance subsidy, consistent with evidence from other similar programmes in India (Shaikh et al. 2018, Kaur et al 2020). Females account for 45% of hospital visits under insurance and this is particularly low among children under 10 years (33%) and the elderly (43%) (Figure 1, Panel A).
Could this be explained by lower illness prevalence among females? Using gender-specific illness prevalence estimates from the Global Burden of Disease (GBD) study for India, we show that across a range of conditions the female share of BSBY hospital visits is 4-10 percentage points lower than projected based on population prevalence (Figure 1, Panel C). We estimate roughly 225,000 missing female hospital visits for nephrology, cardiology, and oncology care alone between 2017 and 2019 due to gender differences in care-seeking.
As a result of these disparities, public expenditure favours males: females accounted for only 44.4% of total programme spending in 2019. Strikingly, the gender gap in insurance utilisation does not decrease over the first four years of the programme, even as increased awareness and enrolment of new hospitals led a to a threefold increase in total programme usage. In other words, simply expanding the programme and encouraging use of it did not reduce disparities.
Figure 1: Gender disparities in BSBY hospital usage
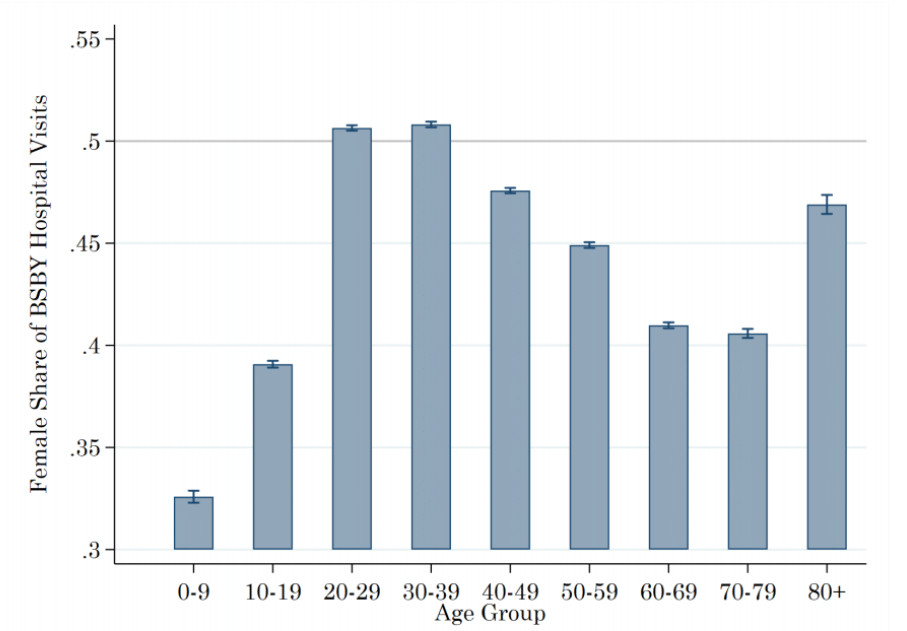
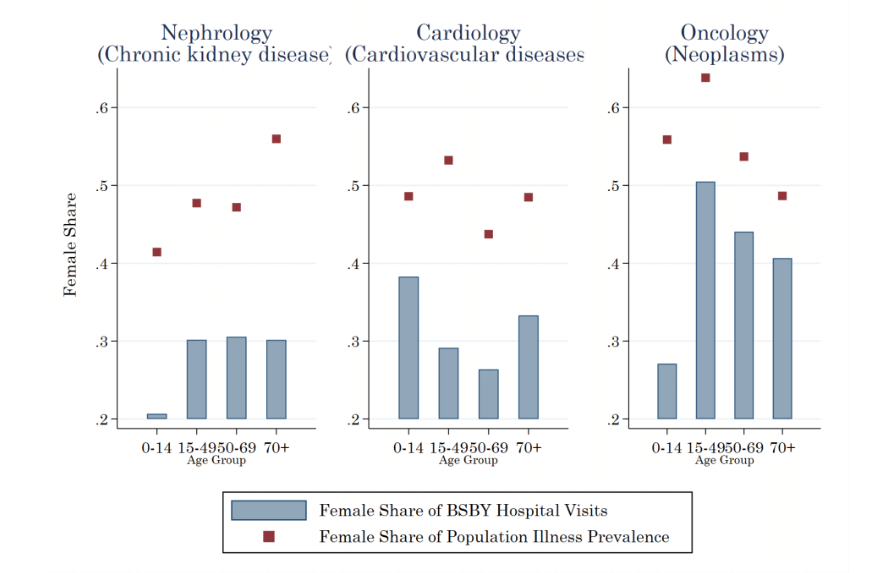
Notes: The figure provides descriptive evidence on gender disparities in BSBY care-seeking. Panel A shows the female share of total BSBY hospitalisations by age group. Females account for only 45% of hospital visits overall, 33% of visits among children under 15yrs, and 43% among adults over 50yrs. Panel B shows that differences in illness prevalence cannot explain the gaps: the female share of BSBY hospitalisation (blue bars) is substantially lower than the female share of illness in the population (red diamonds) across a range of conditions and ages.
Finding 2: Gender disparities increase with care costs
Next, we show that although the programme promises free hospital care, this is not the case in practice, and care costs are associated with larger gender gaps. Surveys we conducted with thousands of recent BSBY users show that 37% faced unauthorised out-of-pocket (OOP) charges by hospitals. Combining this with claims data reveals that the higher the OOP charges for a hospital or service, the less likely females are to use it.
We also study how disparities change with distance to the hospital, another measure of care-seeking costs (Figure 2). Every 10 km increase in the distance from a census location to the nearest BSBY hospital is associated with 3.5% decrease in the female share of BSBY visits from that location. We also see large distance differentials among children, suggesting that the mobility barriers adult women face in India are not the sole explanation for these gaps and that households are willing to allocate fewer resources to female care.
Figure 2: Higher travel costs associated with larger gender disparities

Notes: The figure shows how male and female BSBY visits change as the distance from a village or town to the nearest BSBY hospital increases. Every 10 km increase in the distance from a census location to the nearest BSBY hospital is associated with a 3.5% decrease in the female share of BSBY visits from that location. This relationship persists in regressions with a large set of location controls and is present among patients of all ages, including children.
Finding 3: Reducing care costs does not reduce gender disparities
The descriptive evidence so far already suggests that expanding access to subsidised care is not enough to reduce gender disparities. We take advantage of an administrative reform that enrolled more hospitals in locations with previously limited BSBY coverage to study the causal effect of expanding access and reducing care costs. A 20km (60%) decrease in distance to the nearest eligible hospital led to a 16% increase in female visits in the following year but did not reduce the gender gap because male visits also increased (by 19%, Figure 3). The gap remains unchanged almost two years later.
The intuition behind this is as follows: Increasing subsidies may induce some households to start obtaining care for females in addition to males, thus raising female levels of use. However, it may also induce new households to use BSBY but only for males (reaching their females would require an even larger subsidy). The net effect of a gender-neutral subsidy that can benefit both males and females on disparities (female share of use) depends on which type of households it induces to participate. In a context where many males are not getting care and gender bias is present, a large share of households may continue to allocate subsidies more towards males than females.
Figure 3: Impact of reducing distance to hospitals on female and male visits

Notes: The figure shows the effect of the addition of a BSBY-eligible private hospital near a census location on the number of quarterly male and female BSBY hospital visits from that location. The vertical line represents the date the hospital was enrolled into BSBY. On average, a 20km (60%) reduction in the distance to the nearest private hospital increased female visits by 16% and male visits by 19% with no reduction in gender disparities over the following year.
Finding 4: Directly targeting females reduces the gender disparities
Finally, we examine whether policies that directly target the position of women can improve the effectiveness of the BSBY subsidy. We study the impact of fifteen years of randomised reservations for women in elected village councils (“Gram Panchayats” or GPs) responsible for local public goods and health and education services on BSBY. Each five-year reserved electoral term increases the female share of BSBY visits by 0.9 to 1 percentage points (1.6-3%) among women of childbearing age and children, but there is no effect among the elderly.
Previous work has demonstrated that exposure to female political leaders can reduce gender biases and increase investments in females (Beaman et al. 2009, Beaman et al. 2012, Bhalotra and Clots-Figueras 2014). Consistent with this, we find greater investments in maternal and child health by female leaders, and increased female health worker contacts and agency in reserved villages. In other words, reservations shifted the factors specifically lowering female utilisation rather than gender-neutral reductions in BSBY care costs and barriers.
Social subsidies are unlikely to close disparities without gender-targeted efforts
The key insights from this research extend beyond healthcare to gender inequalities in social services more broadly. While important for expanding access, gender-neutral subsidies may increase female usage of social services but are unlikely to close gender disparities because males benefit as much or more. Larger subsidies that do not substantially reduce gender gaps also mean a large share of public funding is subsidizing males that would have afforded services anyway. Ensuring social programmes reach females and addressing inequalities in outcomes will require gender-targeted strategies that address the specific cost and barriers females face as well as their position in society.
More work is required to understand and address the specific barriers women face in accessing healthcare. However, broader policies targeting women’s mobility and agency, such as free public transport for women, political representation, and changing gender attitudes in school may also have complementary effects on gender inequalities in social programs (Dhar et al. 2021).
References
Anderson, S and D Ray (2010), "Missing women: age and disease", The Review of Economic Studies, 77(4): 1262-1300.
Dhar, D, T Jain, and S Jayachandran (2021), "Reshaping Gender Attitudes: Evidence from Schools in India", VoxDev. Available at: https://voxdev.org/topic/education/reshaping-gender-attitudes-evidence-schools-india (Accessed: 14 February 2024).
Beaman, L, R Chattopadhyay, E Duflo, R Pande, and P Topalova (2009), "Powerful women: does exposure reduce bias?", The Quarterly Journal of Economics, 124(4): 1497-1540.
Beaman, L, E Duflo, R Pande, and P Topalova (2012), "Female leadership raises aspirations and educational attainment for girls: A policy experiment in India", Science, 335(6068): 582-586.
Bhan, N and P P Shukla (2023), "Improving healthcare access to address the rise in non-communicable diseases among Indian women", Ideas for India. Available at: https://ideasforindia.in/topics/human-development/improving-healthcare-access-to-address-the-rise-in-non-communicable-diseases-among-indian-women.html (Accessed: 14 February 2024).
Bhalotra, S and I Clots-Figueras (2014), "Health and the political agency of women", American Economic Journal: Economic Policy, 6(2): 164-97.
Dupas, P and R Jain (2024), ‘Women Left Behind: Gender Disparities in Utilization of Government Health Insurance in India’, Working Paper.
Kaur, S, N Jain, and S Kumar (2020), "Addressing gender issues under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) in India: implications for equity", Working Paper 005, National Health Authority.
Shaikh, M, S A E Peters, M Woodward, R Norton, and V Jha (2018), "Sex differences in utilisation of hospital care in a state-sponsored health insurance programme providing access to free services in South India", BMJ Global Health, 3(3): e000859.


