
Psychotherapy and peer workshops in rural Kenya significantly decreased unhealthy drinking among men while improving agricultural outcomes
Alcohol abuse continues to be a global health problem, and studies link excessive alcohol consumption to many economic, public health, and societal problems, including liver and heart disease, fatal accidents, cancer, and intimate partner violence (Moss 2013).
Sub-Saharan Africa (SSA) is particularly afflicted by alcohol, as alcohol consumption in the region is 20% greater than the global average (WHO 2018). A factor that increases the complexity of the problem in SSA is the widespread consumption of informally produced (i.e. homemade) alcohol. Cheaper than commercial alternatives, this source of alcohol is unregulated, highly potent, and sometimes dangerous given the potential to be contaminated with methanol or additives to increase its potency. In Kenya, the location of this study, this informal alcohol is technically illegal but it remains by far the most common form of alcohol consumed in rural areas, limiting the ability of the government to decrease alcohol consumption using supply-side levers.
Psychotherapy for reducing alcohol consumption
It turns out that there are very few studies in economics on outcomes from effective interventions to decrease alcohol consumption. Most of these use natural experiments tied to alcohol prohibitions (e.g. Luca et al. 2015, Nakaguma and Restrepo 2018, Law and Marks 2020, Khurana and Mahajan 2022). On the demand side, Schilbach (2019) finds commitment devices tied to sobriety in an urban Indian sample are successful in decreasing drinking during working hours. In the medical field, Nadkarni et al. (2017) shows promising results of psychotherapy on alcohol abstention in a primary care setting in India. In the economics literature, however, there has yet to be research analysing the efficacy of psychotherapy and pharmacotherapy programmes on decreasing alcohol consumption and improving economic outcomes.
Details of intervention
To determine the effectiveness of psychotherapy programmes in a rural developing country context, we implemented an intervention as part of a randomised control trial that utilised Motivational Enhancement Therapy (MET) (Miller and Rollnick 1992). This method has been proved to be effective in treating alcohol addiction (Rosenthal et al. 2007) and is similar to the protocol implemented in India by Nadkarni et al. (2017). We also included a nurse on staff who visited and prescribed withdrawal medication when necessary to those in the treatment group. This intervention diverges from previous alcohol programmes, however, by implementing the psychotherapy sessions in a household, rather than clinical, setting and analysing medium-run results (i.e. 16 months) for both alcohol consumption and economic outcomes. Because participants are from rural villages in western Kenya, most are smallholder farmers and we collect both pre- and post-intervention agricultural data.
Enumerators conducted short baseline surveys in late 2020 in thirty randomly selected villages of Bungoma, Busia, and Kakamega countries. From these thirty villages, we received lists from chiefs and village elders of all households with cohabiting spouses in which both spouses were 55 years old or younger. After randomly setting ten villages as a “pure control” in which no intervention activities would take place, the remaining households were randomly assigned to the treatment or set as a “spillover control” group.
Therapists trained in MET began implementing the programme in the twenty treatment villages in February, 2021. The intervention began in each village with three full days of group workshops, in which all households assigned to the treatment in a given village were invited to attend. These workshops focused on the sharing of individual and family challenges associated with alcohol use, developing peer support networks for decreasing alcohol consumption, and the discussion of topics such as peer pressure and family impacts of alcoholism. Following these group workshops, the counselors visited households assigned to the treatment at least eight times over 2-3 weeks for multiple-hour personal and spousal psychotherapy sessions. In these sessions, the therapists employed MET and developed personal and family goals related to reducing alcohol consumption. Spousal therapy included sessions designed to empower spouses in checking each other’s alcohol consumption and strategies to manage urges, such as joint agricultural work. Participation in the programme was relatively high, with 89% of those assigned to the treatment participating in at either the group workshops or psychotherapy sessions, and 75% participating in both.
The intervention reduces harmful drinking
An analysis of a survey with respondents 16 months after the intervention show a significant reduction in harmful drinking behaviour (Murphy 2023). As part of the survey, enumerators asked respondents about the amount of alcohol consumed over the week prior to the survey, collecting data on type, size, and quantity consumed of the beverage. They also asked questions to gauge the maximum amount of alcohol consumed in a single day, as a measure of binge drinking. To guard against potential demand effects (i.e. dishonesty) in answers by the respondent, we separately, privately, and concurrently asked their spouse about both their own and their spouse’s alcohol consumption. I convert all alcohol measures to US standard drink equivalents for comparison.
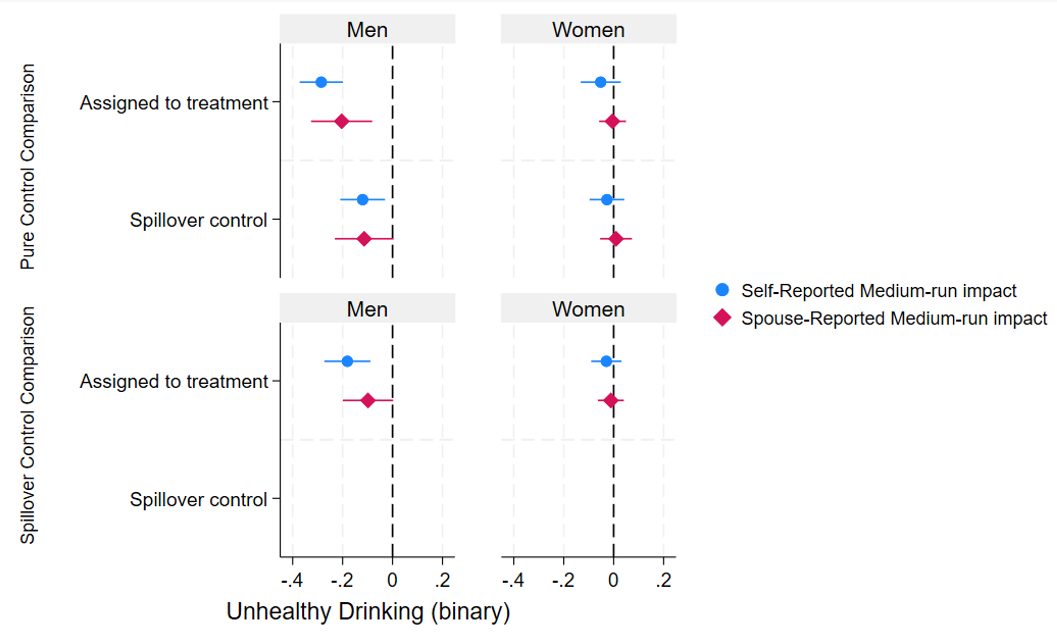
I find that assignment to the treatment reduces the maximum number of drinks consumed in a given day among men by 2.6 US standard drinks (p<.001), relative to a mean in the pure control of 5.8 drinks, using self-reported data (Figure 1). Using spouse reported data, I find a decrease of 1.8 drinks (p<.001), compared to a pure control group mean of 5.1. Among women, there are no effects, which is not surprising given women consume significant less alcohol in this context then men. Figure 2 shows results of the intervention on likelihood of engaging in unhealthy drinking, defined as consuming at least 15 standard drinks in a week for men, or 8 for women. The results show that assignment to the treatment decreases the likelihood of a man being a heavy drinker by 29 percentage points (p<.001) using self-reported data and 20 percentage points using spouse reported data (p<.05) compared to the pure control group, where 54% of pure control group men are heavy drinkers (68% using spouse reported data). As is evident in both figures, after sixteen months, there appears to be some spillover effects to other households in the villages, although the bottom panel of the figures show that in most cases, the effect among the treatment is still statistically significant when compared to those in the spillover control group.
Figure 1: Reduction in number of drinks consumed in a single day
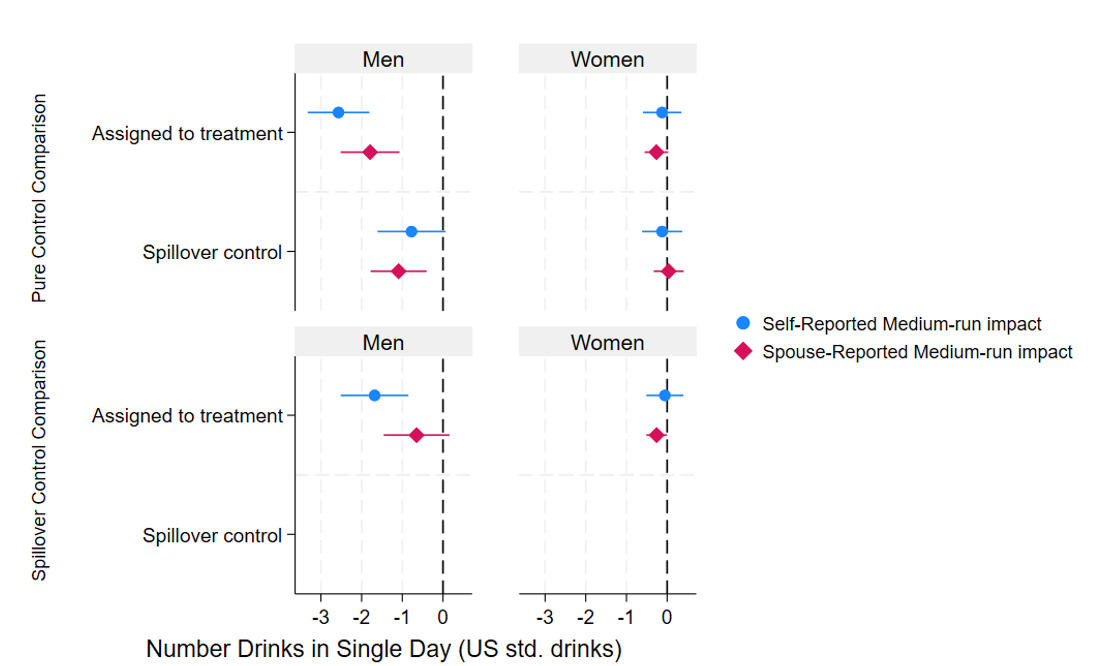
Figure 2: Reduction in likelihood of unhealthy drinking
Effects on economic outcomes
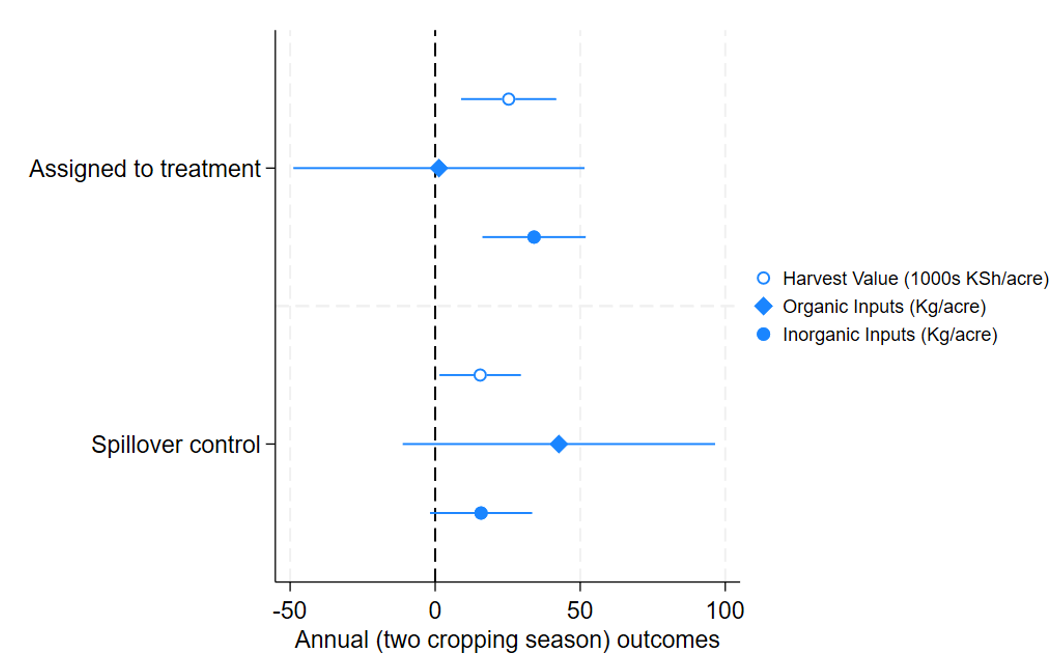
I also analyse the effects of the programme on several different economic outcomes. I find no effects on hours worked (in any sector). I do, however, see effects of the programme on agricultural outcomes. As Figure 3 shows, the intervention led to increases in harvest yields. This is likely caused by greater use of inorganic fertiliser among the treatment. I find evidence that a reallocation of funds from alcohol to agriculture is a likely mechanism, which in turn is likely driven by therapist recommendations, as detail in their notes, to focus on agriculture as a means to control urges to drink.
Figure 3: Agricultural Outcomes
Research implications
As described above, alcohol abuse in SSA is a significant and potentially increasing economic and public health issue. This intervention implemented in western Kenya was relatively inexpensive and has potentially significant effects that appear to be lasting, at least into the medium-run. These results suggest that larger-scale programmes utilising psychotherapy and peer effects can have meaningful effects on substance abuse in the region.
References
Khurana, S and K Mahajan (2022), “Public Safety for Women: Is Regulation of Social Drinking Spaces Effective?” Journal of Development Studies 58(1): 164–82. https://doi.org/10.1080/00220388.2021.1961747.
Law, M and M Marks (2020), “Did Early Twentieth-Century Alcohol Prohibition Affect Mortality?” Economic Inquiry 58(2): 680–97.
Luca, D, E Owens, and G Sharma (2015), “Can Alcohol Prohibition Reduce Violence against Women?” American Economic Review: Papers and Proceedings 105(5): 625–29.
Miller, W and S Rollnick (1992), “Motivational Interviewing: Preparing People to Change Addictive Behavior.” New York: The Guilford Press.
Moss, H (2013), “The Impact of Alcohol on Society: A Brief Overview.” Social Work in Public Health 28(3–4): 175–77.
Murphy, D (2023), “Alcohol, Labor, and Agricultural Productivity.” Working paper. https://dx.doi.org/10.2139/ssrn.3986417
Nadkarni, A, B Weobong, H A Weiss, J McCambridge, B Bhat, B Katti, P Murthy et al. (2017), “Counselling for Alcohol Problems (CAP), a Lay Counsellor-Delivered Brief Psychological Treatment for Harmful Drinking in Men, in Primary Care in India: A Randomised Controlled Trial.” The Lancet 389(10065): 186–95. http://dx.doi.org/10.1016/S0140-6736(16)31590-2.
Nakaguma, M and B Restrepo (2018), “Restricting Access to Alcohol and Public Health: Evidence from Electoral Dry Laws in Brazil.” Health Economics 27(1): 141–56.
Rosenthal, R, K Brady, P Levounis, and M Willenbring (2007), “Advances in the Treatment of Alcohol Dependence.” Journal of Clinical Psychiatry 68(7): 1117–28.
Schilbach, F (2019), “Alcohol and Self-Control: A Field Experiment in India.” American Economic Review 109(4): 1290–1322.
World Health Organization (2018), Global status report on alcohol Global Status Report on Alcohol and Health. http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf%0Ahttp://www.ncbi.nlm.nih.gov/pubmed/29355346.

